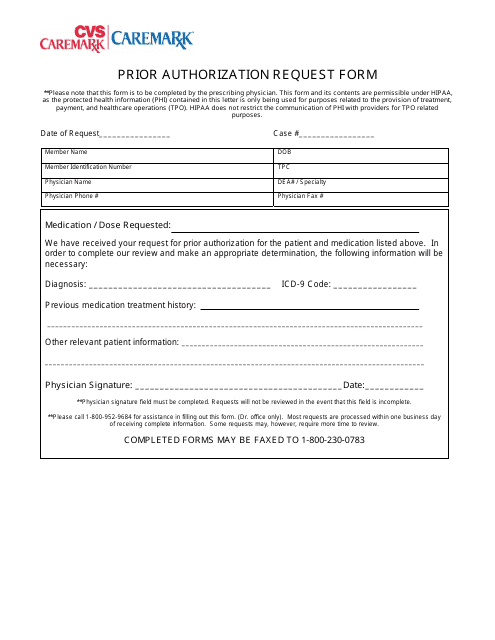
Once a patient or their physician receives a written denial coverage determination they should submit a coverage determination request form asking for the drug to be covered. Please contact CVSCaremark at 1-800-294-5979 with questions regarding the prior authorization process.
 Top Cvs Caremark Prior Authorization Form Templates Free To Download In Pdf Format
Top Cvs Caremark Prior Authorization Form Templates Free To Download In Pdf Format
SilverScript an affiliate of CVS Caremark administers prescription drug benefits for TRS-Care Medicare Rx participants providing predictable copays and convenient delivery options.
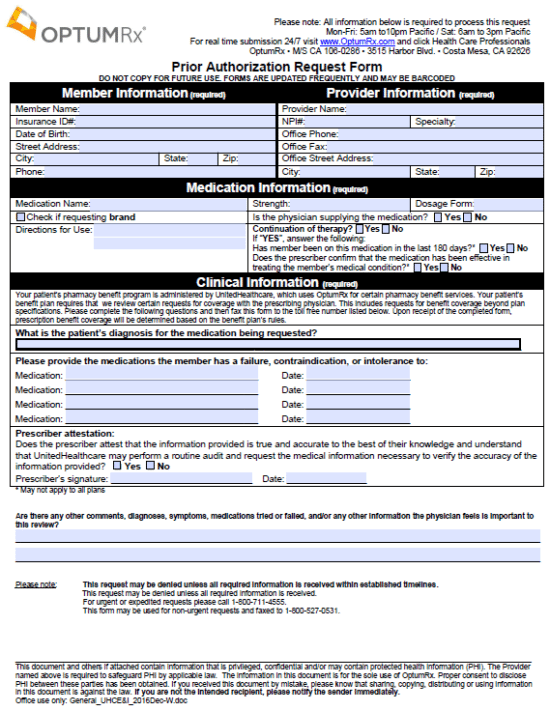
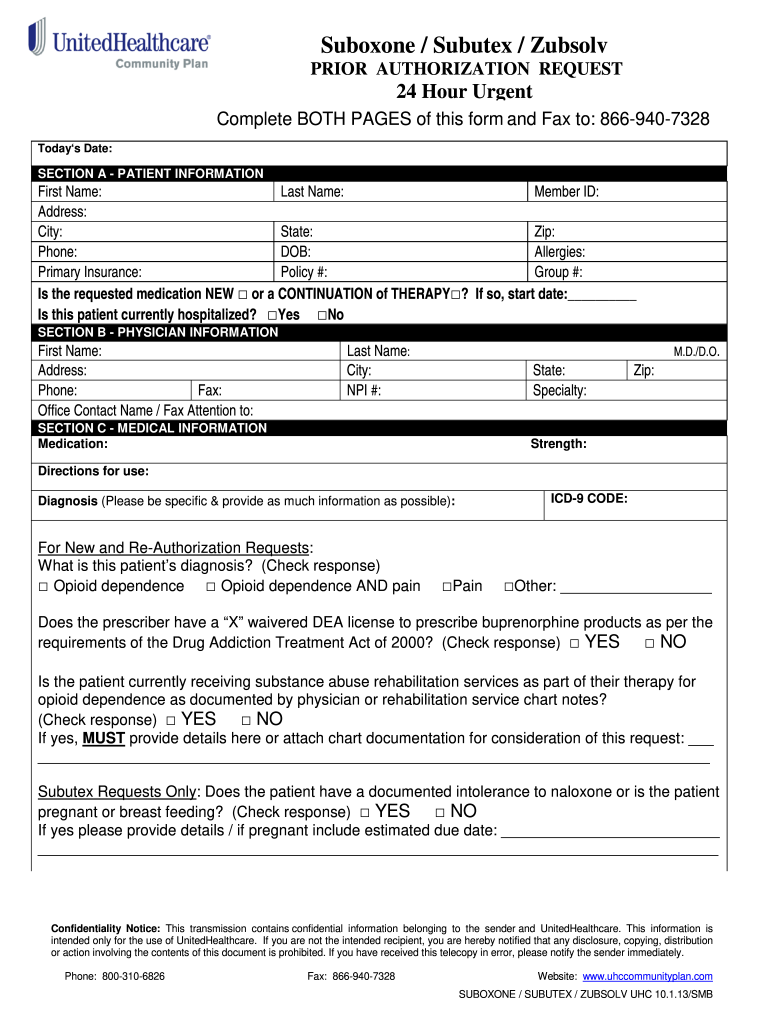
Cvs caremark prior authorization form medicare. In the meantime to send PA please or call the numbers below. This means they process your prescription drug claims. Medicaid PA Request Form.
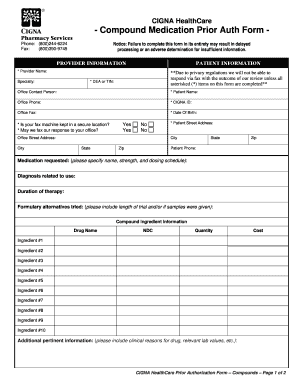
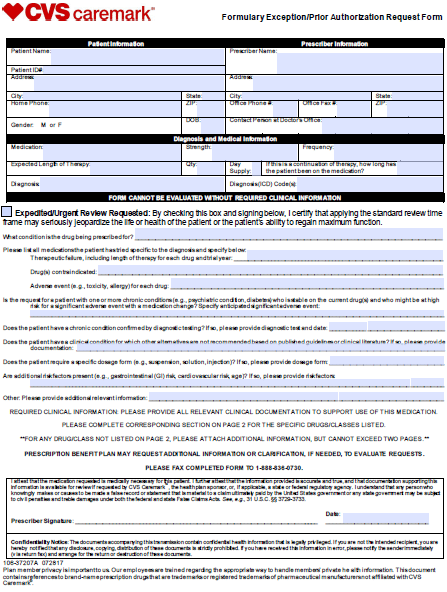
Completereview information sign and date. Contains references to brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with CVS Caremark. CVS Caremark is the Pharmacy Benefits Manager and mail order vendor for MVPs Medicare Advantage plans with prescription drug coverage.
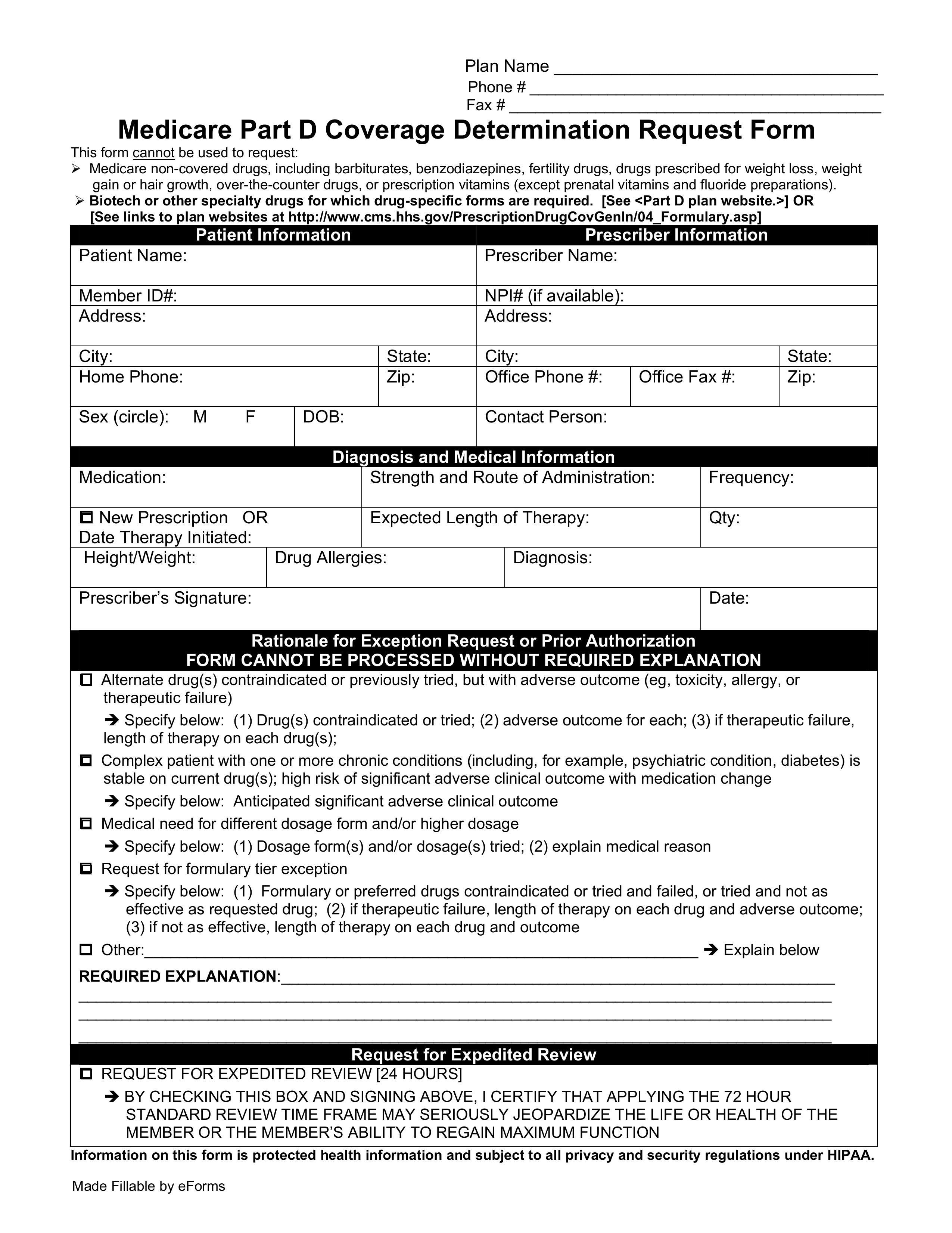
For more information on appointing a representative contact your plan or 1-800-Medicare 1-800-633-4227 TTY. Cvs caremark prior authorization form for testosterone cvs care mark form aetna cvs caremark before covermymeds authorization form before the authorization form pdf cvs caremark before the phone number approves the approval form for medicare cvs caremark before the authorization form for humira cvs caremark pre-application form for adderall cvs. Please provide symptoms lab results with dates andor justification for initial or ongoing therapy or.
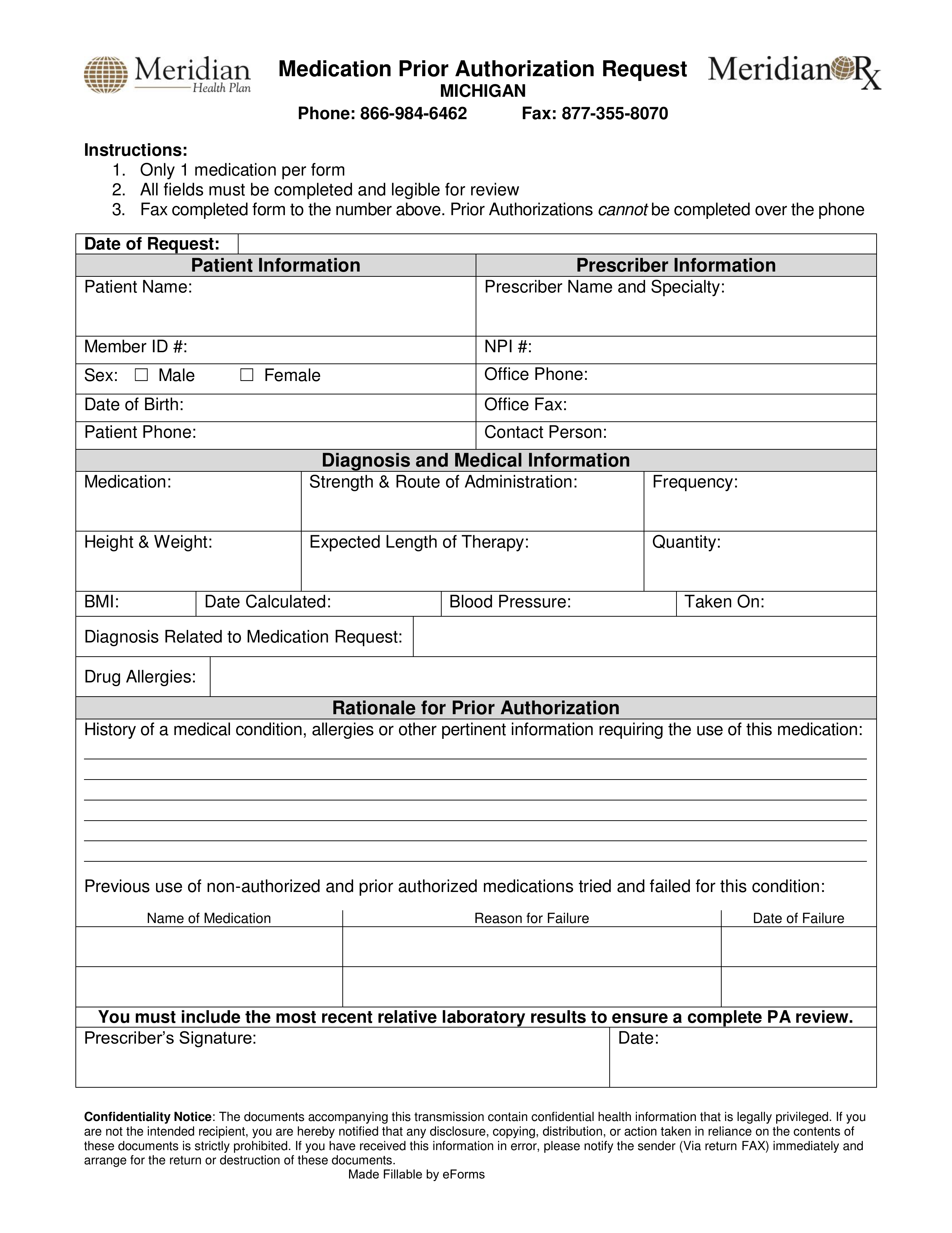
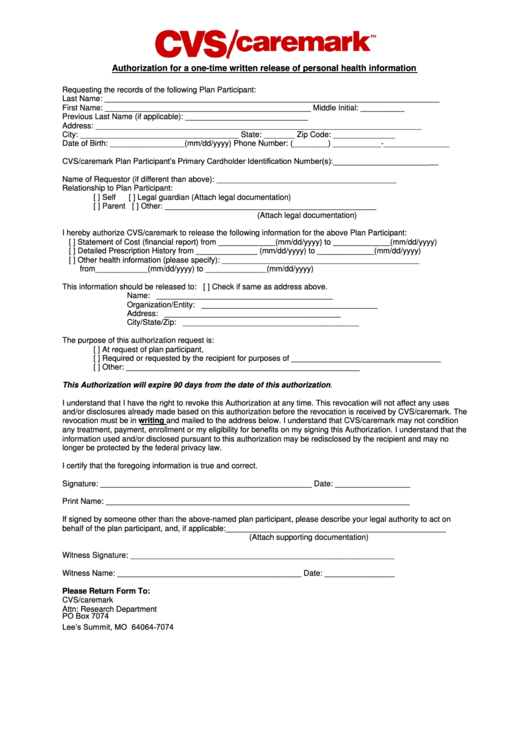
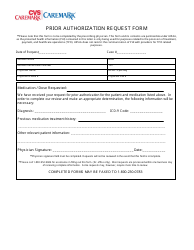
Fax signed forms to CVSCaremark at 1-888-836-0730. A physician will need to fill in the form with the patients medical information and submit it to CVSCaremark for assessment. Fax the completed forms and any supporting documentation to the fax number listed on the form.
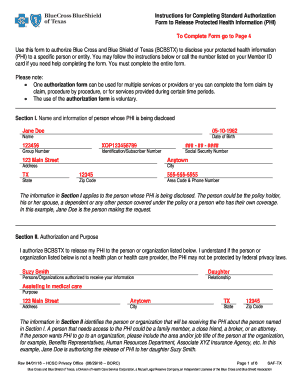
I want to make sure Medicare can give my personal health information to someone other than me Authorization to Disclose Personal Health Information formCMS-10106. A SilverScript prior authorization form is required in order for certain drug prescriptions to be covered by an insurance plan. 1-877-486-2048 24 hours per day 7 days a week.
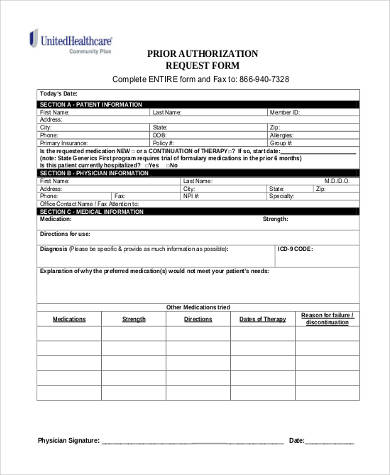
Required clinical information - Please provide all relevant clinical information to support a prior authorization or step therapy exception request review. We are here to help you understand your plan so you can save. Medicaid PA Request Form New York Medicaid PA Request Form.
You can find these forms by selecting Providers from the navigation bar on this page then selecting Forms from the Medicare sub-menu. CVS Caremark provides Medicare information services and tools to help you navigate your plan. Get forms in alternate formats.
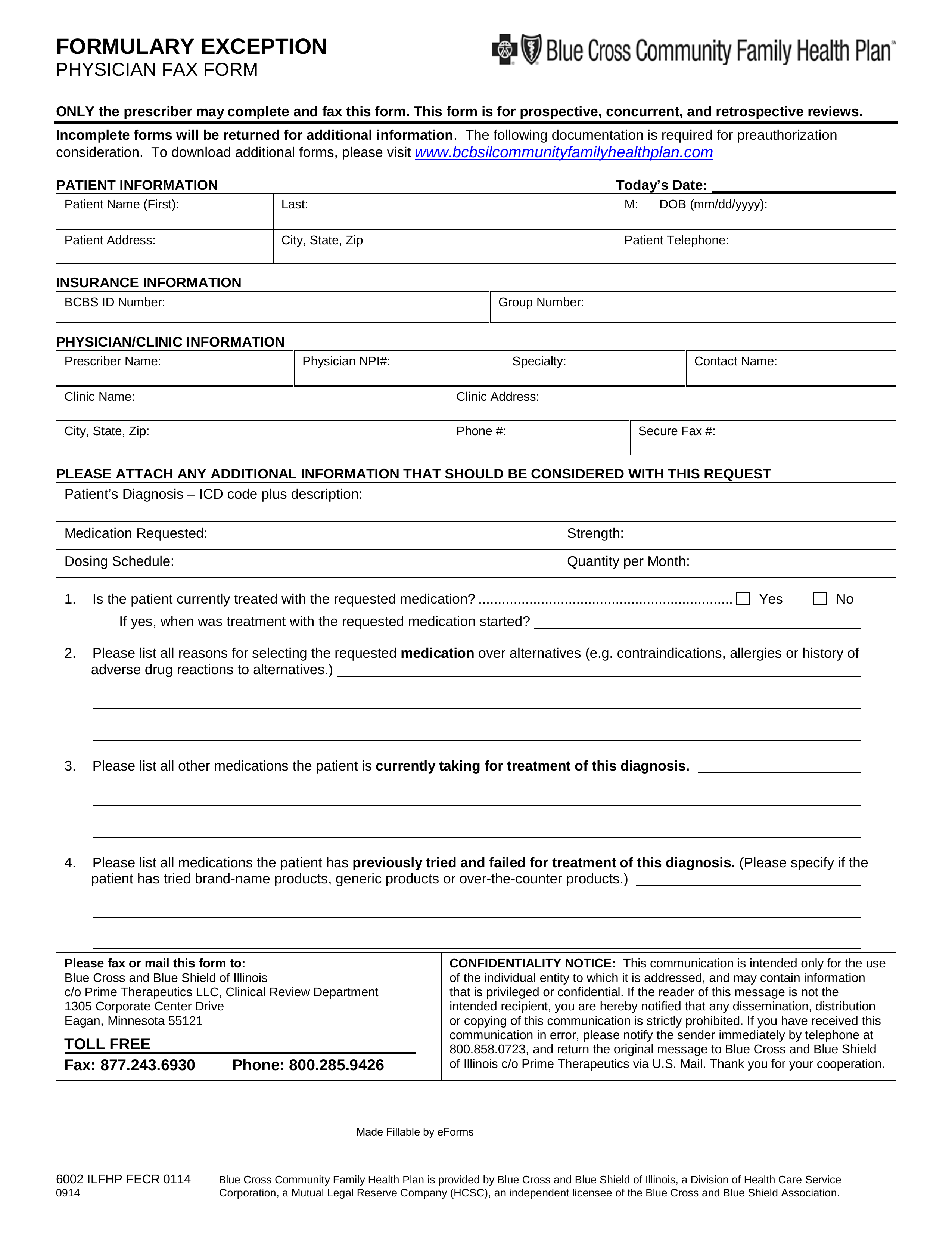
Completereview information sign and date. Request for Medicare Prescription Drug Coverage Determination - Medicare Fill out and submit this form to request prior authorization PA for your Medicare. You do not need to go to a CVSpharmacy for your prescriptionsyou can fill your prescriptions at any pharmacy that contracts with MVP including all major.
Ormulary ExceptionPrior Authorization Request Form Patient Information Prescriber Information Patient Name. Insurance policies have their limitations and in some cases a physician must complete and submit the SilverScript prior authorization form in order to get approval for the drug they intend to prescribe to their patient. Authorization of Representation Form CMS-1696 or a written equivalent.
Get the most out of your Medicare Part D prescription drug plan. Formulary ExceptionPrior Authorization Request Form Patient Information Prescriber Information Patient Name. The CVSCaremark prior authorization form is to be used by a medical office when requesting coverage for a CVSCaremark plan members prescription.
To get the Medicare form you need find the situation that applies to you. Complete the appropriate WellCare notification or authorization form for Medicare. If you wish to request a Medicare Part Determination Prior Authorization or Exception request please see your plans website for the appropriate form and instructions on how to submit your request.
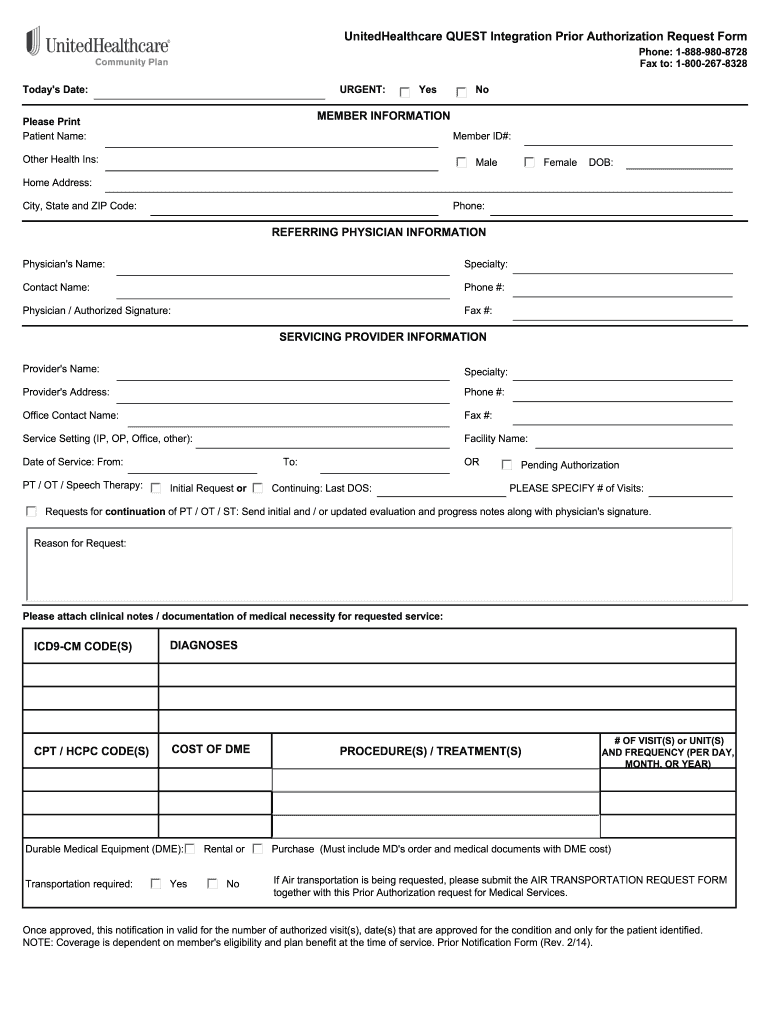
Brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with CVS Caremark. The Medicare Prior Rx Authorization Form or Drug Determination Request Form is used in situations where a patients prescription is denied at the pharmacy. Request Method Commercial QUEST Integration Medicare Electronic PAs Phone 1 855 240-0543 1 855 220-5732 1 855 479.
Prior Authorization Form Isotretinoin Products This fax machine is located in a secure location as required by HIPAA regulations. CVS Caremark Criteria Type. Contact CVS Caremark Prior Authorization Department Medicare Part D.
Prior Authorization Form Amitiza This fax machine is located in a secure location as required by HIPAA regulations. Fax signed forms to CVSCaremark at 1-888-836-0730. Please contact CVSCaremark at 1-855-582-2022 with questions regarding the prior authorization process.
Cvs caremark prior authorization form for livalo CVS Caremark will be updated before the form fax form license is being updated and will be made available soon. Initial Prior Authorization Ref 2634-A Drugs that are listed in the target drug box include both brand and generic and all dosage forms.