There are hundreds of different medications with more becoming available every day. They will also evaluate whether the procedure is medically necessary.
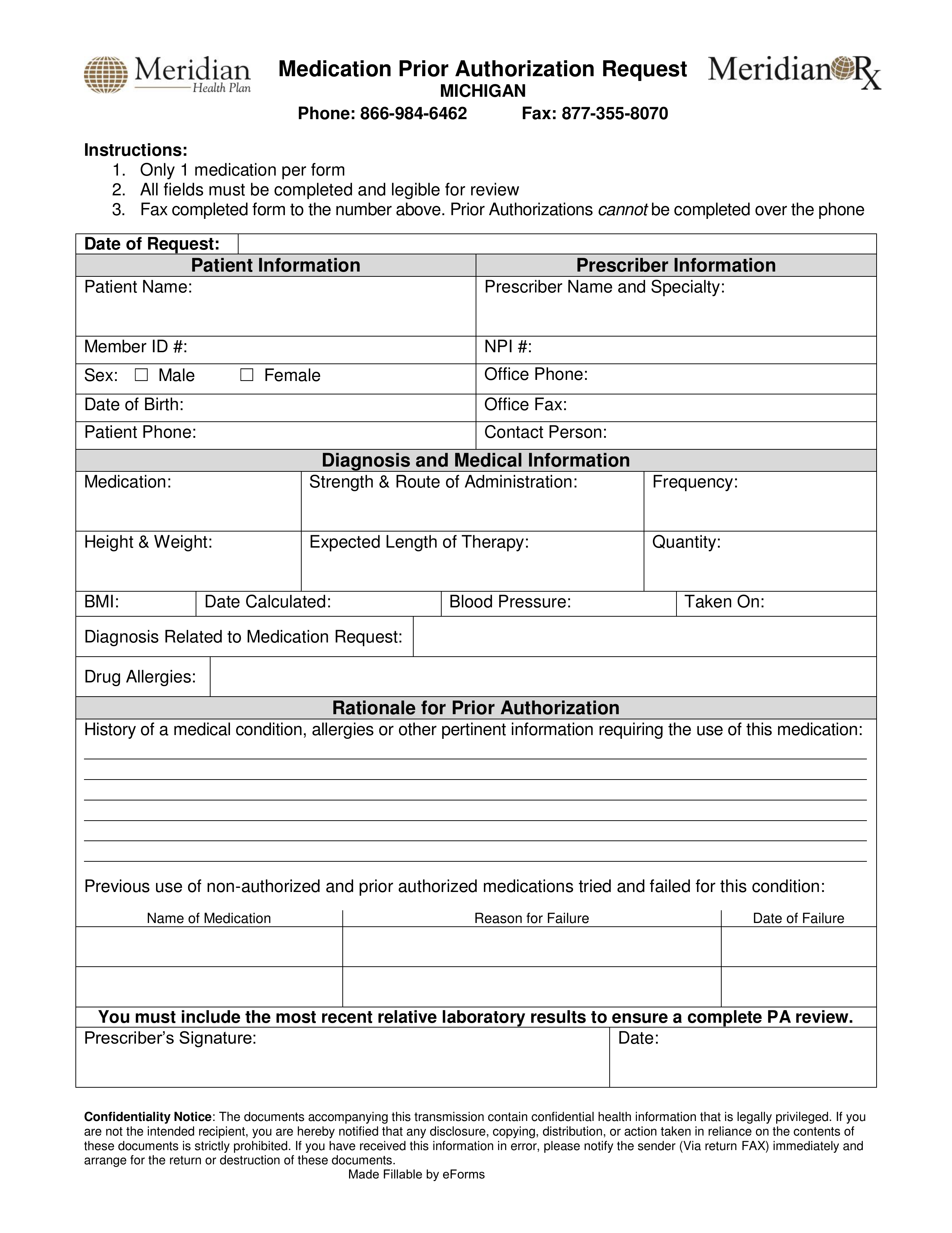 Free Meridian Prior Rx Authorization Form Pdf Eforms
Free Meridian Prior Rx Authorization Form Pdf Eforms
Health insurance companies use prior authorization to verify that a certain drug procedure or treatment is medically necessary before it is done or prescribed.
Prior authorization for medication. How Do I Get Prior Authorization for a Medication. Prior authorization also called prior approval or pre-authorization is a process that many health insurance companies as well as Medicare and Medicaid use to manage costs. Brand-name drugs that have a generic available.
Drugs that are intended for certain age groups or conditions only. You can view the most up-to-date. Drugs that are neither preventative nor used to treat.
When determining prior authorization the insurance company will look at a few things. This information explains what it means if your doctor has prescribed a medication that needs prior authorization. Depending on a patients plan you may be required to request a prior authorization or precertification for any number of prescriptions or services.
Its also a way for your health insurance company to manage costs for otherwise expensive medications. What is prior authorization. Prior authorization is designed to help prevent you from being prescribed medications you may not need those that could interact dangerously with others you may be taking or those that are potentially addictive.
You may find these on. On the prior authorization form the person making the request must provide a medical rationale as to why the chosen medication is necessary for the patient in question. As part of this effort we retired certain fax numbers for medical prior authorization requests in 2019 and asked you to use the Prior Authorization and Notification tool on Link the same website you use to check eligibility and benefits manage.
Your pharmacy will contact if your doctor if he or she did not obtain prior authorization from the insurance. Drugs used only for cosmetic reasons. Prior authorization PA is often used with expensive prescription drugs.
Services requiring advance notification and prior authorization vary by plan and can change. Start date of service. Without this prior approval your health insurance provider may not pay for your medication or operation leaving you with the bill instead.
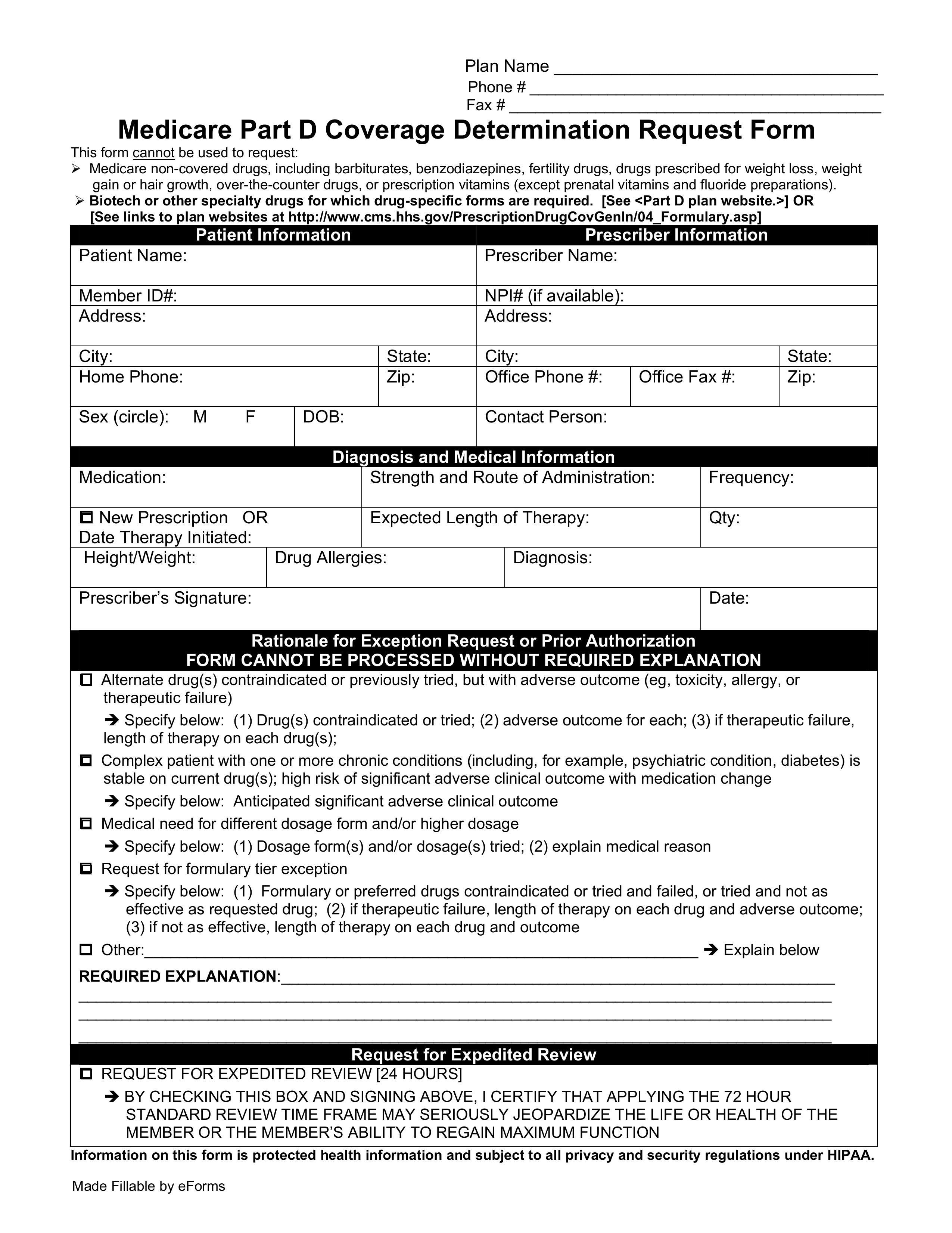
Insurance companies will most likely require prior authorizations for the following drugs. Prior authorizationsometimes called precertification or prior approvalis a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage. Prescription prior authorization forms are used by physicians who wish to request insurance coverage for non-preferred prescriptions.
Blue Cross Blue Shield of Michigan and Blue Care Network use prior authorization to make sure you get the right medication. Your insurance provider. Prior authorization refers to an insurance company not authorizing itself to pay for a medicine prior to its knowing anything about a case.
Service code if available HCPCSCPT. Before you can get coverage for certain medications tests procedures surgeries and medical devices you need to get prior authorization. The bottom line is that insurance companies often have a.
A non-preferred drug is a drug that is not listed on the Preferred Drug List PDL of a given insurance provider or State. If a PA is needed locate the process for submitting and obtain any required prior authorization forms. A full list of CPT codes are available on the CignaforHCP portal.
Prior authorization is a requirement that your physician obtains approval from your healthcare provider before prescribing a specific medication for you or to performing a particular operation. How to Get Prior Authorization after the fact. They will look to see whether your specific plan covers the procedure hospital and doctor.
This form is to be completed by the patients medical office to see if he or she qualifies under their specific diagnosis and why the drug should be used over another type of medication. The Medicaid prior authorization forms appeal to the specific State to see if a drug is approved under their coverage. Insurance companies are referred to as health care which is deceptive.
This evaluation includes a review of your medical history including what alternative treatments youve already tried. Services requiring prior authorization require a clinical coverage review based on medical necessity. Check your plans policy documents and formulary to see if any of your treatments require a PA.
If the patient has tried any preferred medications. The physician will contact the insurance company and submit a formal authorization request. Policies may vary between each states department of health but the process more.
End date of service.
 Prior Authorization Form Free Word Templates Prior Authorization Consent Letter Sample Letter Form
Prior Authorization Form Free Word Templates Prior Authorization Consent Letter Sample Letter Form
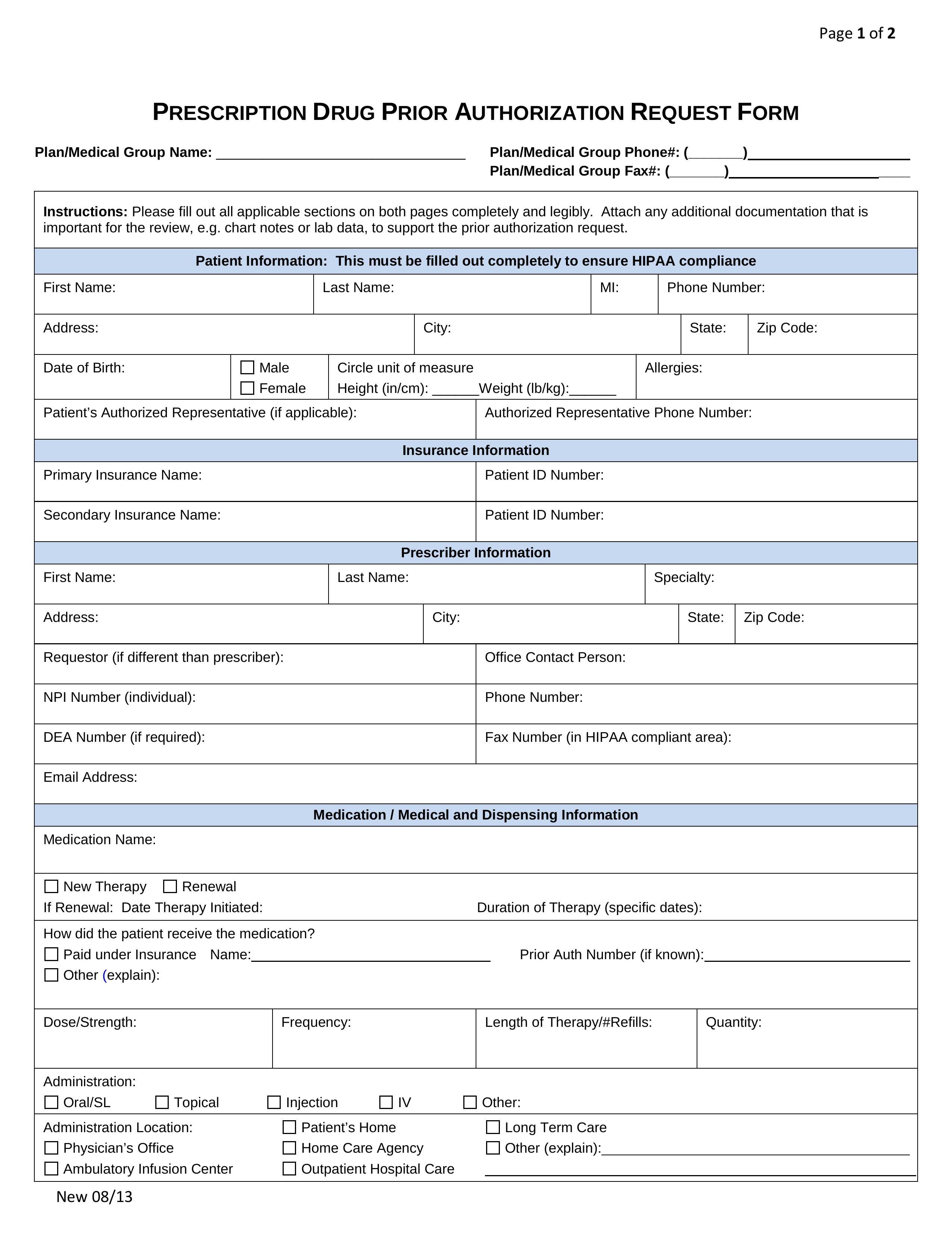 Free Prior Rx Authorization Forms Pdf Eforms
Free Prior Rx Authorization Forms Pdf Eforms
 Fillable Online Medication Prior Authorization Form Fax Back To 18775779045 Member Information Last Name Phone 18775779044 D Fax Email Print Pdffiller
Fillable Online Medication Prior Authorization Form Fax Back To 18775779045 Member Information Last Name Phone 18775779044 D Fax Email Print Pdffiller
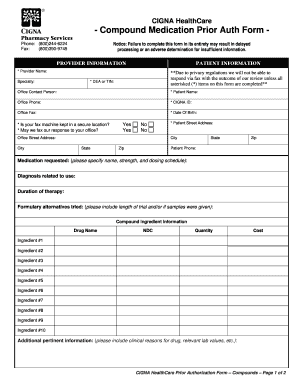
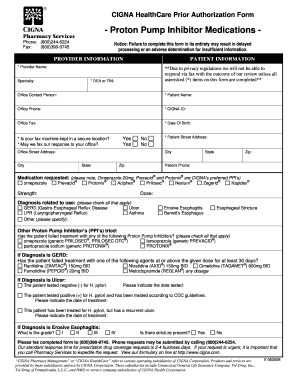
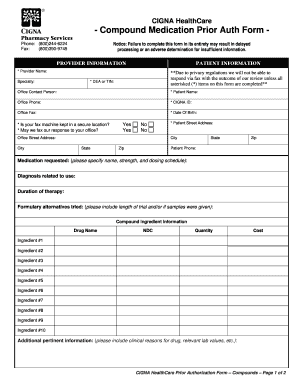 20 Printable Cigna Authorization Forms Templates Fillable Samples In Pdf Word To Download Pdffiller
20 Printable Cigna Authorization Forms Templates Fillable Samples In Pdf Word To Download Pdffiller
 Oh No My Prescription Requires A Prior Authorization Now What Don T Fill Your Prescription
Oh No My Prescription Requires A Prior Authorization Now What Don T Fill Your Prescription
 Free 9 Sample Prior Authorization Forms In Ms Word Pdf
Free 9 Sample Prior Authorization Forms In Ms Word Pdf
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
 Surescripts Medication Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Surescripts Medication Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
![]() Oh No My Prescription Requires A Prior Authorization Now What Don T Fill Your Prescription
Oh No My Prescription Requires A Prior Authorization Now What Don T Fill Your Prescription
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
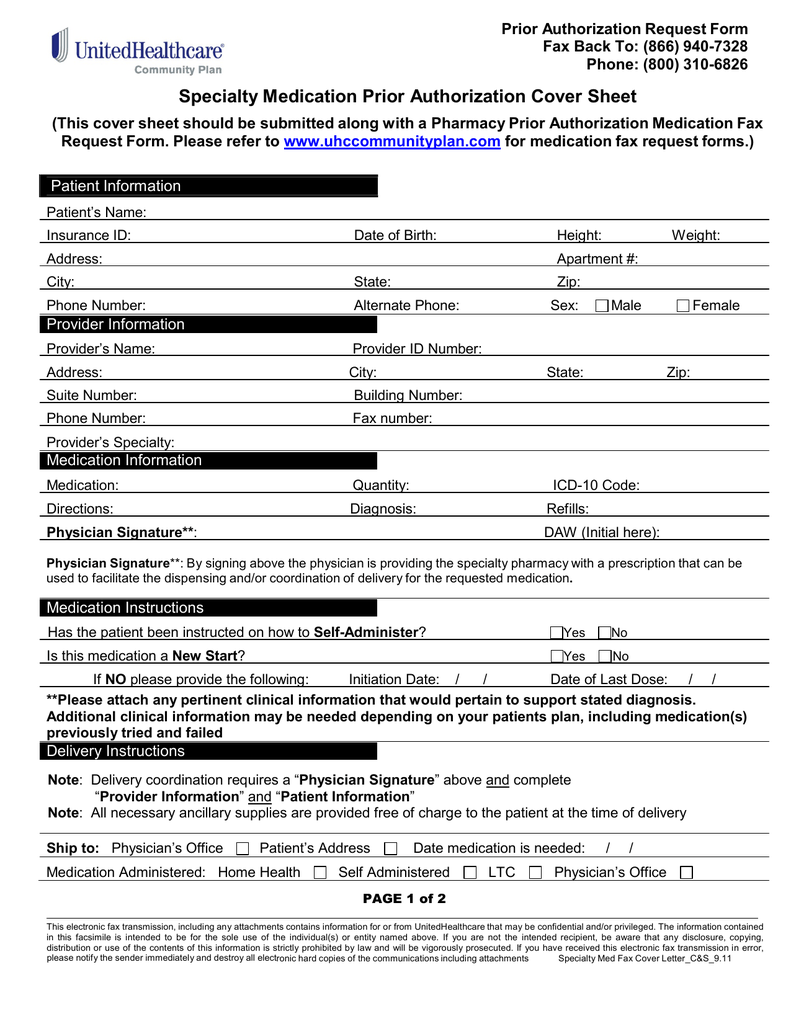 Specialty Medication Prior Authorization Cover Sheet
Specialty Medication Prior Authorization Cover Sheet
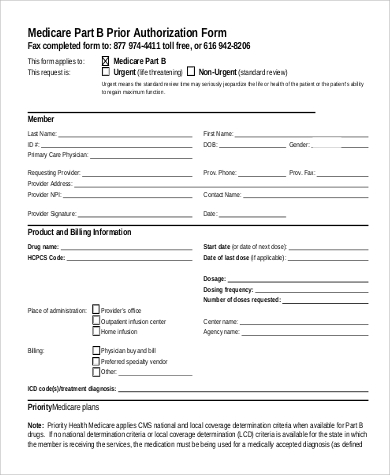
 Free Medicare Prior Rx Authorization Form Pdf Eforms
Free Medicare Prior Rx Authorization Form Pdf Eforms
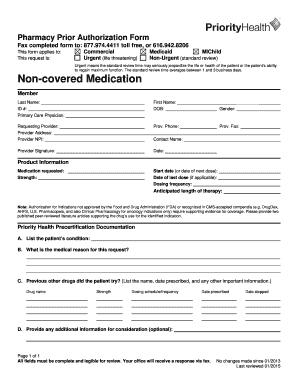 Priority Health Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Priority Health Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.