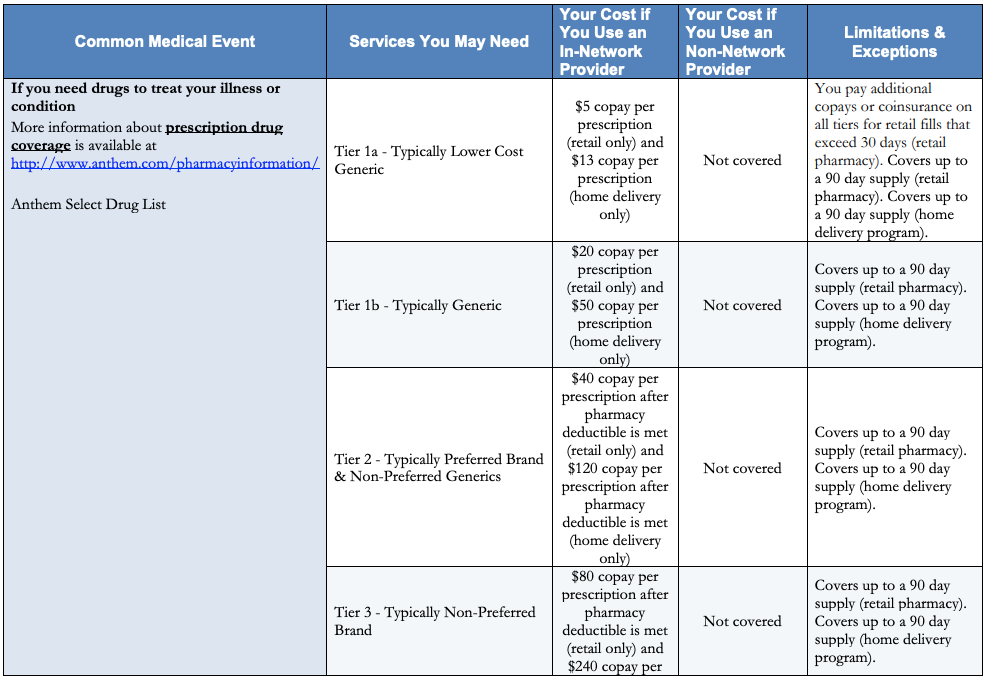
Prices do not include federal state or local taxes or additional fees. Discounts on All Prescription Drugs.
 Prescription Drug Prices Global Comparison To Us 2018 Statista
Prescription Drug Prices Global Comparison To Us 2018 Statista
Prices quoted may not be exact as there can be multiple manufacturers with varying costs for the same medication.
Medication price finder. Below is a list of resources where you can find drug prices. Finding the lowest price available for your prescription should be quick and easy. 231 Zeilen Find out drug price by their brand or through generic names listed alphabetically.
The cost of medication is different from country to country and pharmacy to pharmacy. That led to you having to drive around town to find the lowest price. Price information updated daily.
This material is provided for educational purposes only and is not intended for medical advice diagnosis or treatment. WellRx Price as Low as 2116. Data sources include IBM Watson Micromedex updated 3 May 2021 Cerner Multum updated 4 May.
Print out your discount card and start saving an average of 50 percent on prescription costs. You used to have to call around to find out what the price for your medication was going to be and even then. In Denmark medicines are sold at the same prices from all pharmacies and there is free price formation.
The pharmacist rarely would give you the price of your medication over the phone. Show Your Card or App. Prescription prices may vary from pharmacy to pharmacy and are subject to change.
Compare prescription drug prices and find coupons at more than 70000 US pharmacies. Save up to 80 instantly. Easily find the lowest price for your medication at more than 65000 pharmacies nationwide.
Prices of medicines are fixed by pharmaceutical companies and sold at the same prices from all pharmacies in Denmark. The retail prices displayed above represent estimated prices for your prescription drugs. Show your discount card or use the app at the pharmacy of your choice.
Prices from PharmacyChecker Discounted Card prices in White Plains NY. Department of Veterans Affairs OPAL Federal Supply Schedule. Discounts on brand or generic prescriptions.
To find the lowest drug prices its often essential to compare medication costs locally and internationally. Always seek medical advice from a medical professional for diagnosis or treatment including before embarking on andor changing any prescription medication or for specific medical advice related to your medical history. Savings average 65 and in some cases can be 80 or more.
Prices are retail pharmacy estimates only and are based on typical contracted prices paid to pharmacies. GoodRx Website that tracks US prescription drug prices and offers drug coupons World. Click on a medication to see prices for your locations.
Drug Price Finder Pharmacy Locator. The pricing estimates given are based on the most recent information available and may change based on when you actually. Pharmacy discounts are NOT insurance and are not intended as a substitute for insurance.
This means that prices are fixed by the companies manufacturing or importing the medicines into Denmark. We compare pharmacy prices from more than 57000 participating pharmacies to find you the best discount. Terms of Agreement Privacy Policy.
Save on Your Medications. Top Price Guide Drug Searches. Search for the Lowest Price.
A-Z Index of Price Guide Medications. Centers for Medicare. You can use this calculator to compare prices for your medications to find the best price options in your area using the NeedyMeds Drug Discount Card.
Pharmacy discounts range from 10 to 85 on most medicationsThe discount is only available at participating pharmacies. Finding medicine at discounted prices has never been easier. The Danish Medicines Agency has no impact on the companies price.
An Easy Way to Find Medicine at Discount Prices.