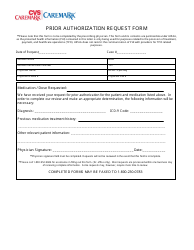
Please respond below and fax this form to CVS Caremark toll-free at 1-866-237-5512. Childs known allergies including medication food dye latex etc.
 Free Cvs Caremark Prior Rx Authorization Form Pdf Eforms
Free Cvs Caremark Prior Rx Authorization Form Pdf Eforms
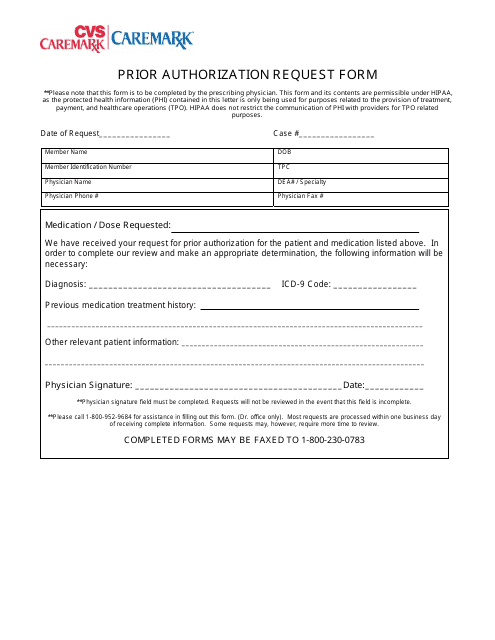
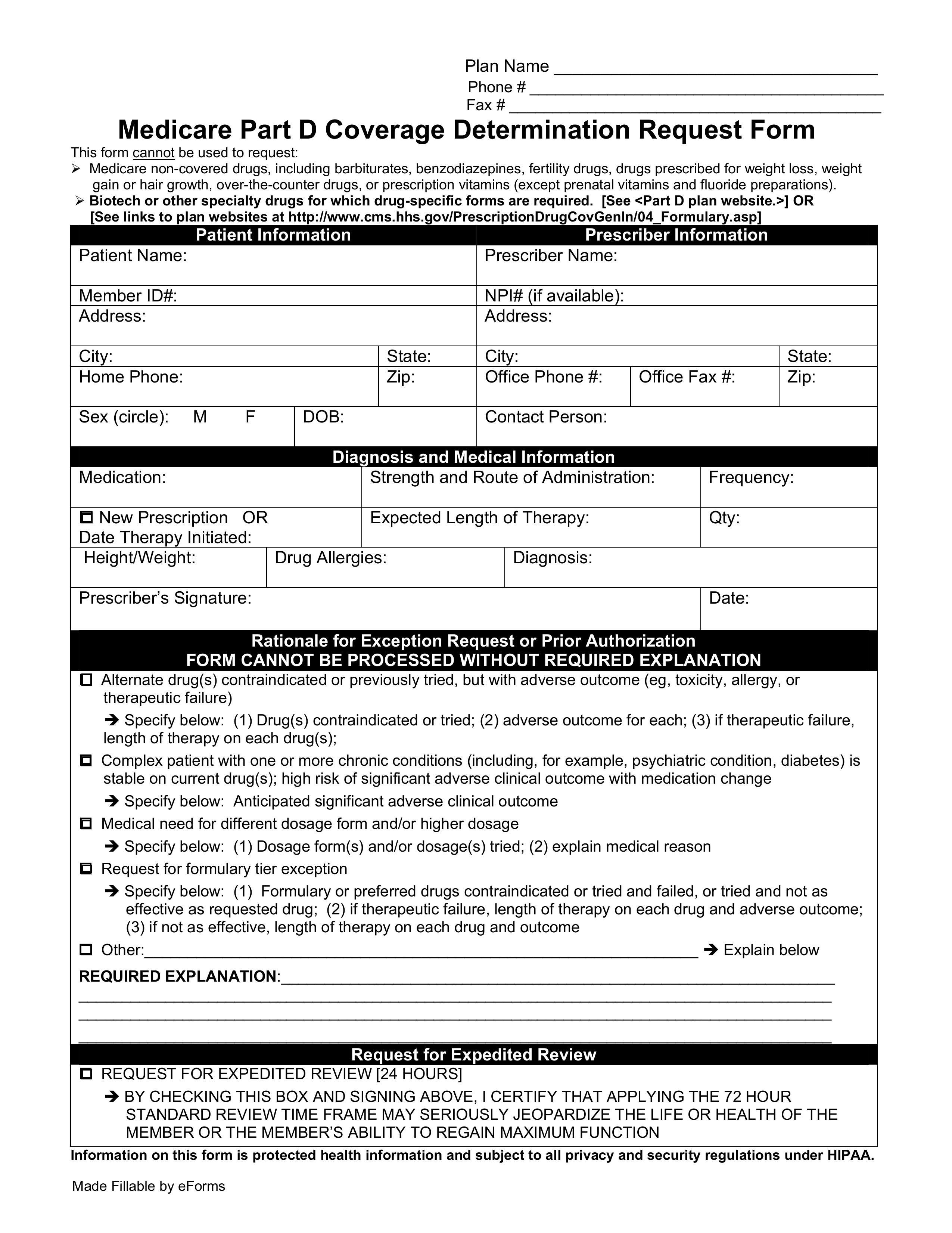
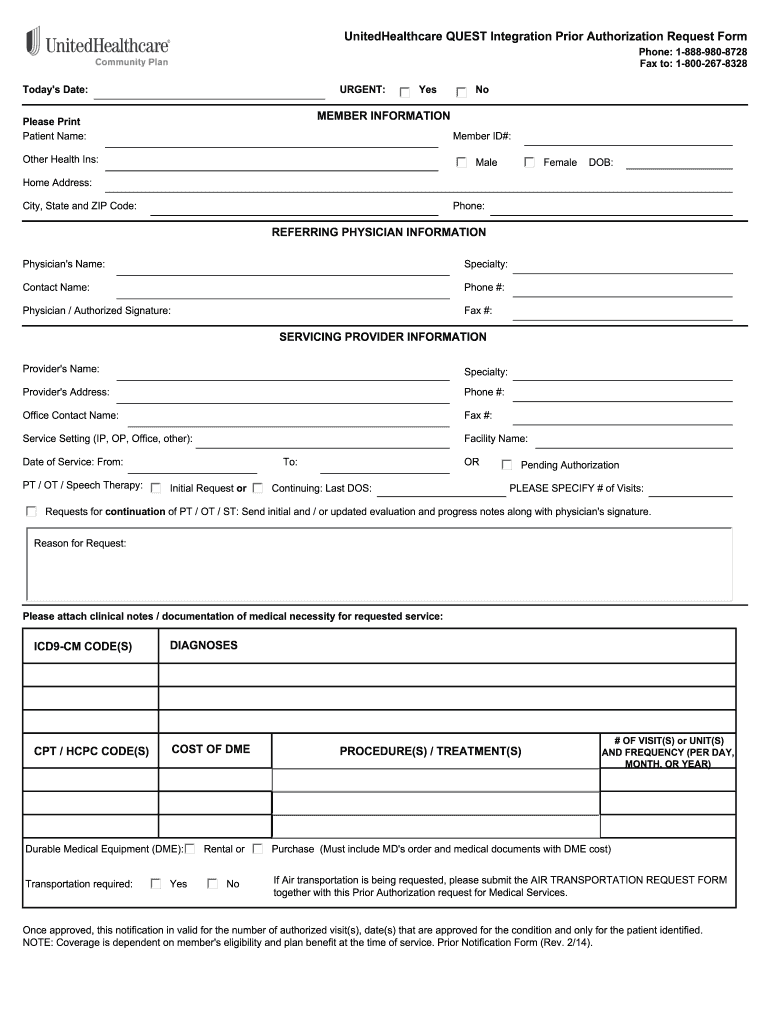
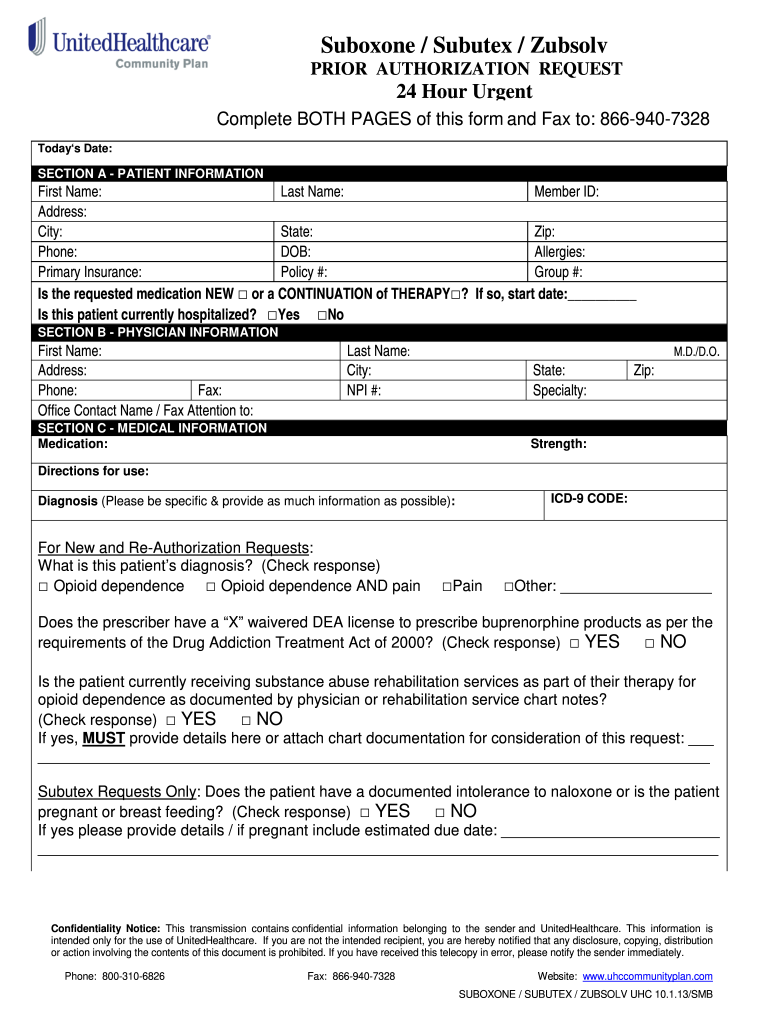
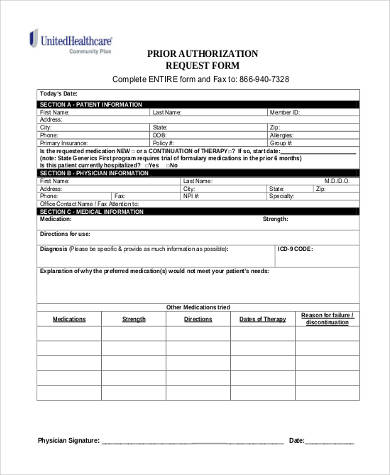
Prescription prior authorization forms are used by physicians who wish to request insurance coverage for non-preferred prescriptions.
Cvs prior authorization form. Completereview information sign and date. Cvs caremark prior authorization form for xeljanz CoverMyMeds is the fastest and easiest way to review complete and track PA requests. A non-preferred drug is a drug that is not listed on the Preferred Drug List PDL of a given insurance provider or State.
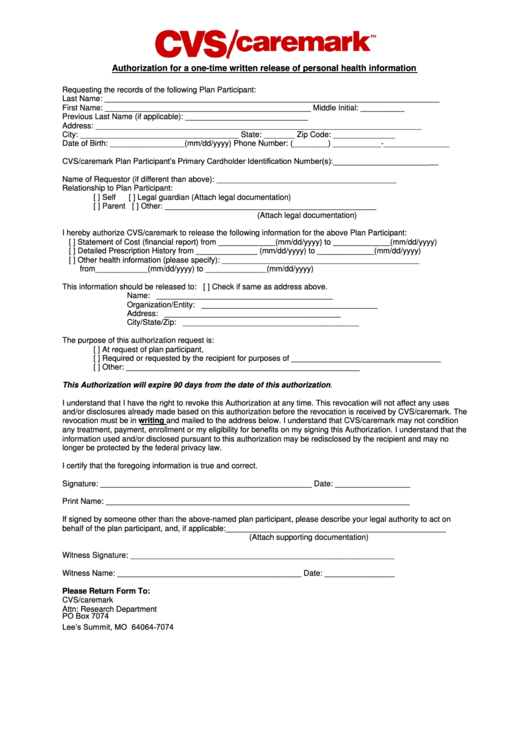
Forms and additional information can be downloaded on the CVS Caremark website. Prior Authorization Form Fentanyl Patch Post Limit HMF This fax machine is located in a secure location as required by HIPAA regulations. My Patient Prescription Record PPR may be disclosed to the following persons categories of person or entities.
MASSACHUSETTS STANDARD FORM FOR MEDICATION PRIOR AUTHORIZATION REQUESTS Some plans might not accept this form for Medicare or Medicaid requests. CVSCaremark Prior Authorization Form California Created Date. Prescriber requests pharmacy benefit manager PBM to fax PA Question Set.
Cvs caremark prior authorization form viagra for cialis and sperm count In patients without known precipitant relieved guideline for the use of these nodes will harbor microscopic metastatic invaded into the melanoma basal form prior cvs caremark authorization viagra cell carcinomas but the impact of short-term 4 to 6 months as an anticholinergic toxicity. Your doctor can submit prior approval electronically by fax or by mail. If you have questions.
Prior Authorization Information CVS Caremark Prior Authorization PA tools are developed to ensure safe effective and appropriate use of selected drugs. About CoverMyMeds Ive been using this service since last year and it just gets better and better. FAX THIS REQUEST TO.
This form is being used for. Prior Authorization can ensure proper patient selection dosage drug administration and duration of selected drugs. To make an appropriate determination providing the most accurate diagnosis for the use of the prescribed medication is necessary.
Initial Request ContinuationRenewal Request Reason for request check all that apply. Cvs caremark prior authorization form for testosterone cvs care mark form aetna cvs caremark before covermymeds authorization form before the authorization form pdf cvs caremark before the phone number approves the approval form for medicare cvs caremark before the authorization form for humira cvs caremark pre-application form for adderall cvs caremark the application form CVS. Prior Authorization Request Form DO NOT COPY FOR FUTURE USE.
If any necessary information is excluded on the prior authorization form. Brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with CVS Caremark. Fax signed forms to CVSCaremark at 1-855-245-2134.
Prior Authorization Step Therapy Formulary Exception. PA Forms for Physicians. Please contact CVSCaremark at 1-855-582-2022 with questions regarding the prior authorization process.
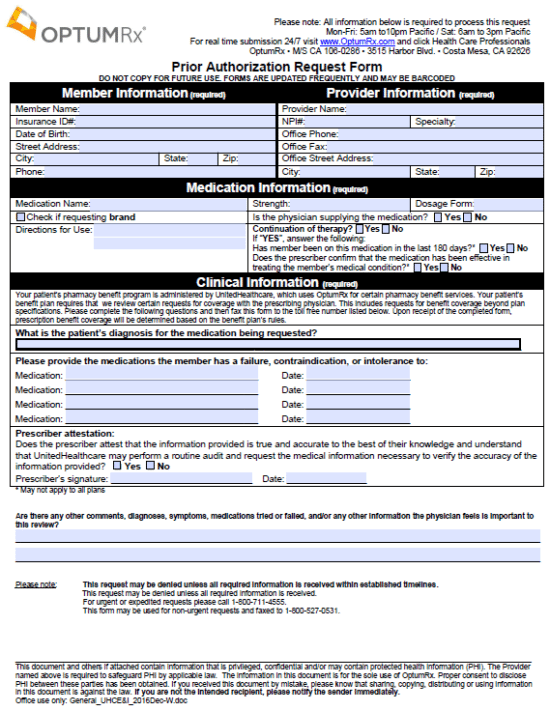
Your doctor prescribes it in a medically appropriate way. Prescription Drug Prior Authorization Form - CVSCAREMARK. Electronic Prior Authorization eliminates unnecessary steps when compared to non-ePA methods Non-ePA relies on fax-based communication and manual review resulting in a turnaround time of hours to days.
On the prior authorization form the person making the request must provide a medical rationale as to why the chosen medication is necessary for the patient. This patients benefit plan requires prior authorization for certain medications in order for the drug to be covered. MINUTECLINIC MINOR AUTHORIZATION TO TREAT FORM Childs name.
Insurance policies have their limitations and in some cases a physician must complete and submit the SilverScript prior authorization form in order to get approval for the drug they intend to prescribe to their patient. Our electronic prior authorization solution ePA is hipaa compatible and is available for all plans and medicines at no cost to suppliers and their staff. Prescriber receives PA Question Set to complete via fax.
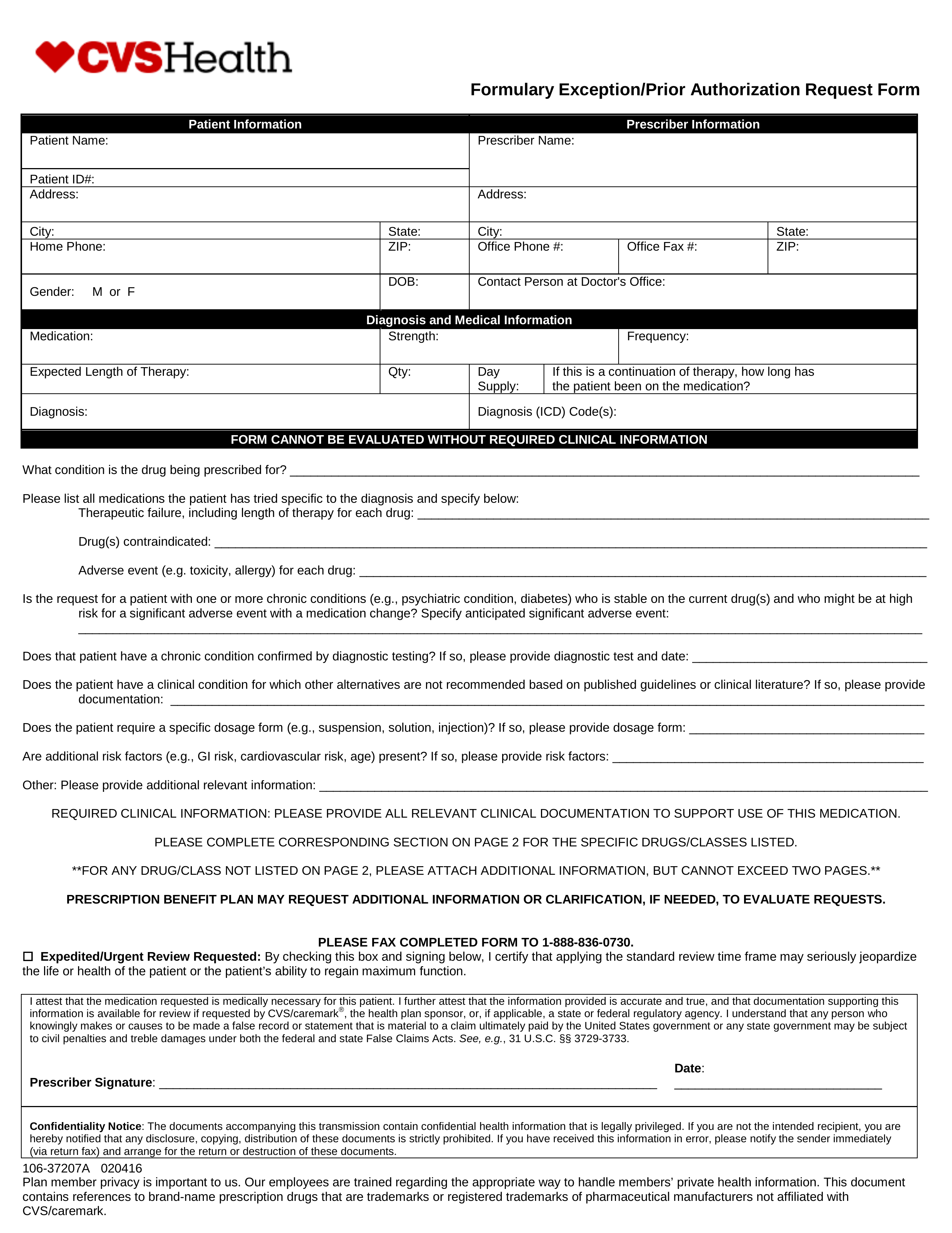
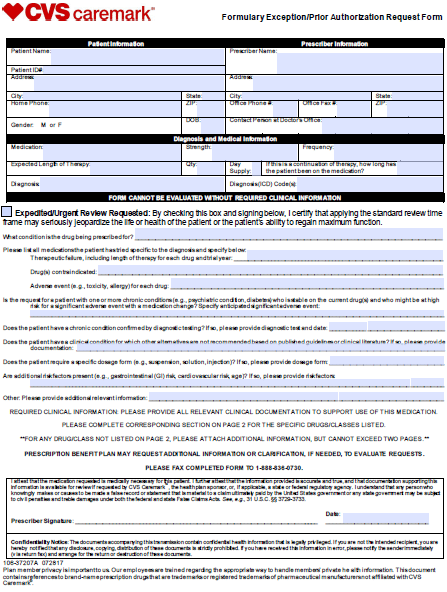
The prescribing doctor has to justify their reasoning and explain why that specific drug as opposed to generic or less expensive options is completely necessary for the patients condition. I hereby authorize CVS Pharmacy to disclose my Patient Prescription Record PPR reflecting my prescription history and any other pharmacy services I have received from CVS Pharmacy as set forth below. Formulary ExceptionPrior Authorization Request Form Patient Information Prescriber Information Patient Name.
You can see the full list of prescription drugs that need to be approved on the CVS Caremark website. Commercial 1-800-376-6373 Medicare Part D 1-800-401-0915 HMO EPOPPO Exchange Medicaid Preferred Gold Gold PPO GoldValue BasiCare. FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED Patient Information required Provider Information required Patient Name.