The AMA believes that the overall volume of medical. You need to contact your regional contractor for prior authorization.
 The Ultimate Guide To Prior Authorization Myndshft
The Ultimate Guide To Prior Authorization Myndshft
Establish a solid insurance verification process for all new and returning patients.

How to obtain a prior authorization. Providers who plan to perform both the trial and permanent implantation procedures using CPT code 63650 in the OPD will only require prior authorization for the trial procedure. Stamp of Approval. As much as you.
If the request is approved by MDHHS this tracking number becomes the prior authorization number to use for billing purposes. How to Obtain Prior Authorization for PT Services 1. Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service.
Prior authorization is a restriction put in place by insurance companies so they can decide whether or not they will pay for certain medicines. Depending on a patients plan you may be required to request a prior authorization or precertification for any number of prescriptions or services. Your dermatologists office creates a request and submits the information required by your insurance provider for prior.
Ordering care providers will complete the notificationprior authorization process online or over the phone. Services requiring prior authorization through BCBSTX Medical Management Submit via Authorizations Referrals an online tool in the Availity Provider Portal. You may find these on.
If you have a referral then your provider gets prior authorization at the same time. Labs must register their tests to participate as part of the Genetic and Molecular Lab Testing NotificationPrior Authorization process. If youre not required to get referrals you should know what services need prior authorization.
Learn more about the Genetic Molecular Lab Testing Notification Prior Authorization Process. Prior authorizationsometimes called precertification or prior approvalis a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage. On this call we will outline the process for submitting a prior authorization request to your designated Durable Medical Equipment Medicare Administrative Contractor DME MAC the timeframes for the DME MAC to render their prior authorization decisions and the process for subsequent claim submissions.
The physician will contact the insurance company and submit a formal authorization request. Prior authorization is a process through which a request for provisional affirmation of coverage is submitted for review before the service is rendered to a beneficiary and before a. You can call or register on your contractors site for secure services.
Steps for getting prior authorization Your dermatologist writes a prescription. Get really familiar with your payers authorization processes and guidelines paying special attention to your top. Getting prior authorization means youre getting the care approved by your regional contractor before you actually go to an appointment and get the care.
Your pharmacy will contact if your doctor if he or she did not obtain prior authorization from the insurance. Youll get an authorization letter after its approved. After your prescription is sent to the pharmacy by your dermatologist or.
How to Get Prior Authorization after the fact. Once the PA request is successfully entered the provider receives a tracking number. A full list of CPT codes are available on the CignaforHCP portal.
Prior Authorization is about cost-savings not care. One of the following profiles is needed to access the PA tab. DMEPOS suppliers and other participants will be encouraged to submit questions and.
Obtain prior authorizationprenotification as follows. Under Prior Authorization benefits are only paid if the medical care has been pre-approved by Medicare. If a PA is needed locate the process for submitting and obtain any required prior authorization forms.
Check your plans policy documents and formulary to see if any of your treatments require a PA. How Do I Get Prior Authorization for a Medication. It doesnt affect cash payment for prescriptions and its only required on those prescriptions when billed through insurance so if youre uninsured or if you decide to pay in cash you wont need to worry about getting prior authorization.
Private for-profit plans often require Prior Authorization. The only service that will require prior authorization for implanted spinal neurostimulators is CPT code 63650. How to request precertifications and prior authorizations for patients.
When the trial is rendered in a setting other than the OPD providers will need to request prior authorization for. To learn more visit Availity Authorizations Referrals. CHAMPS Full Access CHAMPS Limited Access Prior Authorization Access.
 Why Automation Is The Key To Fixing Prior Authorization Myndshft
Why Automation Is The Key To Fixing Prior Authorization Myndshft
How To Obtain Health Insurance Prior Authorization In 3 Minutes Or Less
 16 Tips To Dramatically Speed Up Prior Authorizations
16 Tips To Dramatically Speed Up Prior Authorizations
 Prior Authorization Problems Preempt Them By Leveraging Software
Prior Authorization Problems Preempt Them By Leveraging Software
 How To Obtain Prior Authorizations Jdrf
How To Obtain Prior Authorizations Jdrf
 The Ultimate Guide To Prior Authorization Myndshft
The Ultimate Guide To Prior Authorization Myndshft
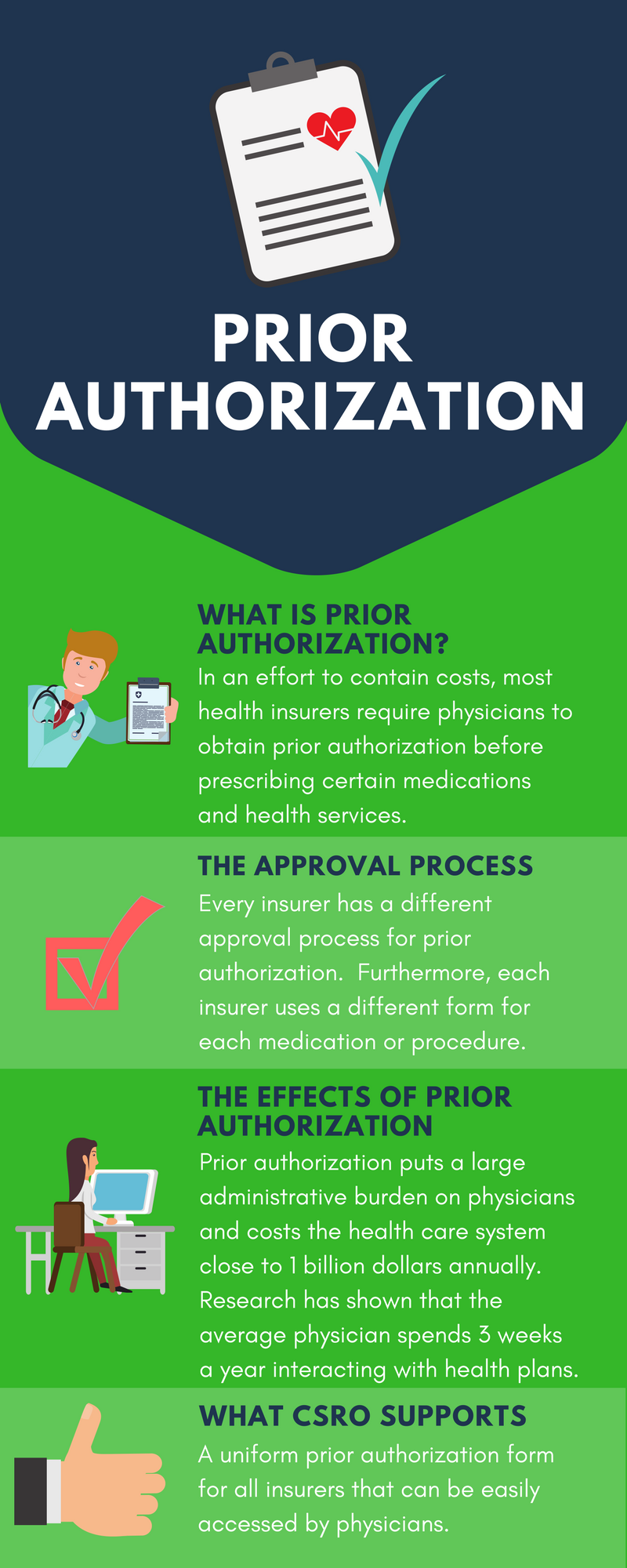 Coalition Of State Rheumatology Organizations Uniform Prior Authorization
Coalition Of State Rheumatology Organizations Uniform Prior Authorization
 Importance Of Preauthorization In Revenue Cycle Management Rcm
Importance Of Preauthorization In Revenue Cycle Management Rcm
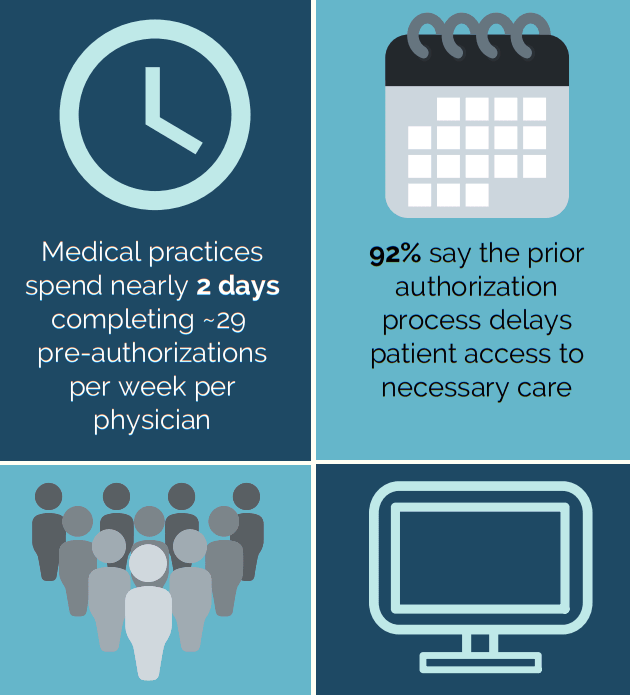
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 Pre Authorization And Pre Certification
Pre Authorization And Pre Certification
 Importance Of Preauthorization In Revenue Cycle Management Rcm
Importance Of Preauthorization In Revenue Cycle Management Rcm
 Eligibility Benefits Verification And Prior Authorization Services
Eligibility Benefits Verification And Prior Authorization Services
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 How To Get Medical Pre Approval Or Prior Authorization Effectively
How To Get Medical Pre Approval Or Prior Authorization Effectively
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.