Please only submit one preauthorization per form. There are two ways to initiate your request.
 2020 Texas Standard Prior Authorization Request Form For Health Care Services Fill Out And Sign Printable Pdf Template Signnow
2020 Texas Standard Prior Authorization Request Form For Health Care Services Fill Out And Sign Printable Pdf Template Signnow
When prior authorization is required you can contact us to make this request.
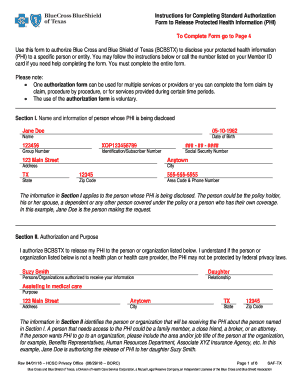
Bcbs prior auth form. Use this form to request authorization by fax or mail when a n issuer requires prior authorization of a health care service. An Issuer may also provide an electronic version of this form on its website that you can complete and submit electronically through the issuers portal to request prior authorization of a health care service. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
Use Get Form or simply click on the template preview to open it in the editor. 17 Zeilen Behavioral Health for Other BCBSTX Plans. Prior Authorization Request for Medically Necessary Orthodontia Services for Pediatric Essential Health Benefits Psychological and Neuropsychological Assessment Supplemental Form Use this supplemental form as a cover sheet for the standardized Mass Collaborative form.
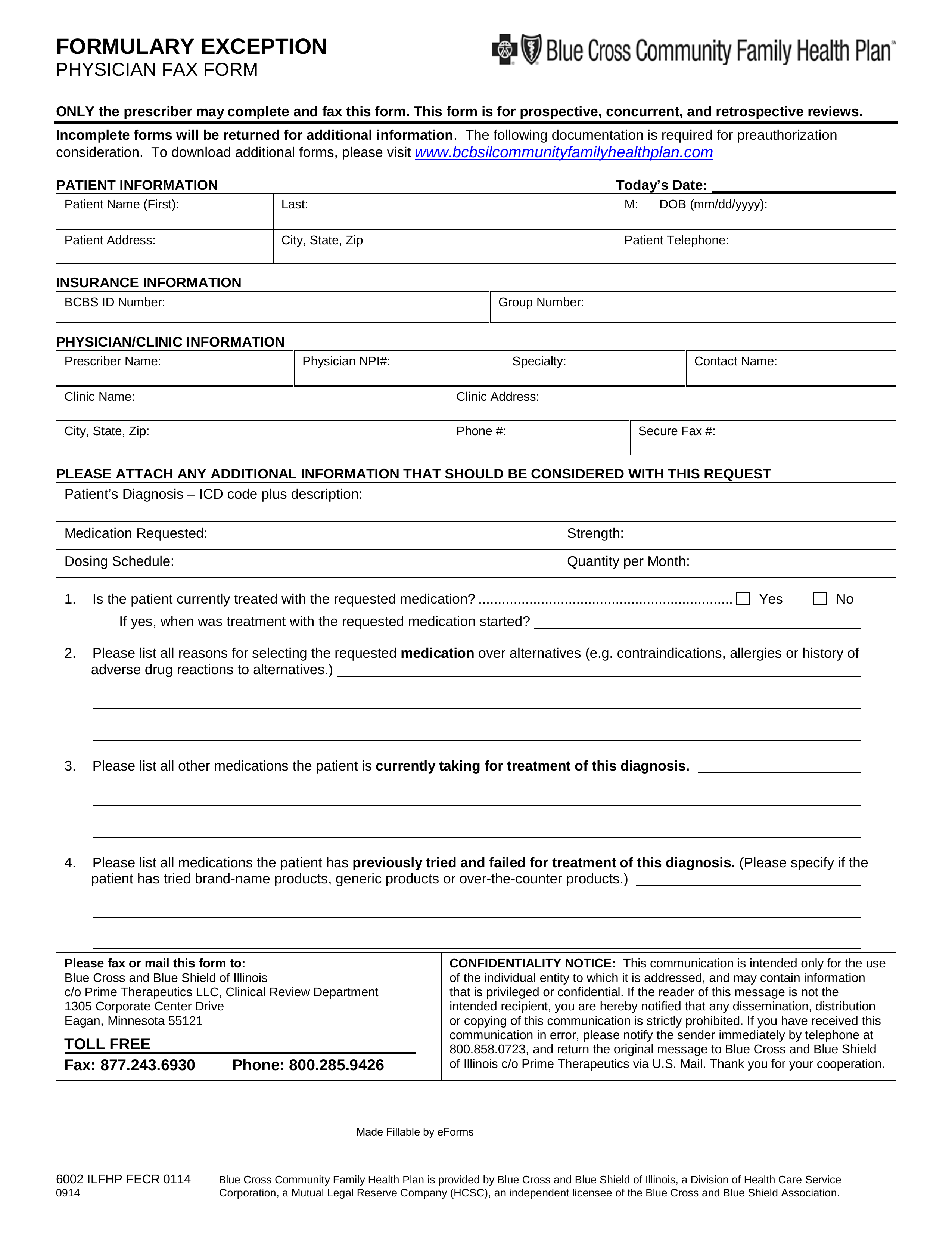
Fax request Complete the Preauthorization Request form or the NM Uniform Prior Authorization Form and submit it along with your supporting documentation Telephone Inquiries Call the preauthorization number on the back of the members ID card. Online Prior Authorization Form PDF forms are available below to submit a prior authorization. For some services listed in our medical policies we require prior authorization.
Affordable Care Act Forms PDF You can also submit prior authorization requests using these specific forms. Durable Medical Equipment Certification Form. For ERS or TRS participants refer to.
Some services require prior authorization preauthorization before they are performed. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. Medical Transport Prior Approval Request.
Mental Health Prior Authorization. We use established clinical guidelines to confirm medical necessity when your health plan requires prior authorization. Or call our Health Services department at.
For instructions refer to the Availity Authorizations User Guide. Start completing the fillable fields and carefully type in required information. Urgent Request Non-urgent Request.
Post Service - Ambulance Trip Sheet Form. YBD YBG YBS YBM YBT YBX YJV YJW YJJ or YJT. Use the Cross or Check marks in the top toolbar to select your answers in the list boxes.
Simply click on the form name to open them. Services DME prostheses Radiology Services. Authorization form for appeals on the members behalf Member Appeal Representation Authorization Form New prescription fax order form for PrimeMail Prime Therapeutics - Pharmacy Fax Order Form Form to record your notes from ambulance trips.
Forms to Download PDF format The forms below are all PDF documents. The member ID for someone in an Individual and Family ACA Plan will begin with one of the following prefixes. Include any documents to support your request send a copy of your documents and keep all originals.
Outpatient Prior Authorization CPT Code List 072 Prior Authorization Quick Tips. NYS Medicaid Prior Authorization Form for Prescriptions. For prior authorization requests handled by BCBSIL.
Quick steps to complete and e-sign Aim Specialty Prior Authorization Form online. Obtaining a prior authorization helps us pay claims faster with no denied charges or unexpected costs to our members. To submit a prior authorization online please click the button below to use the web form.
Only life-threatening situations will be considered for urgent requests. Urgentemergency admissions do not require prior authorization. Prior authorization sometimes called pre-certification is how Blue Cross and Blue Shield of Minnesota makes sure the treatment your doctor prescribes is medically necessary and helps ensure you are getting proper care.
Online Registered Availity users may use Availitys Authorizations tool HIPAA-standard 278 transaction. Submit a Transplant Prior Authorization Request. Fax If you would prefer to submit your request by fax complete and follow the submission directions on this form.
Contact Companion Benefits Alternatives CBA to verify by calling 800-868-1032. Health Care Services Referral Form To refer a patient who is a BlueCross BlueShield member to our disease management case management or health coaching service complete and fax this form to the number enclosed. A few plans may continue to require prior authorization for mental health services.
