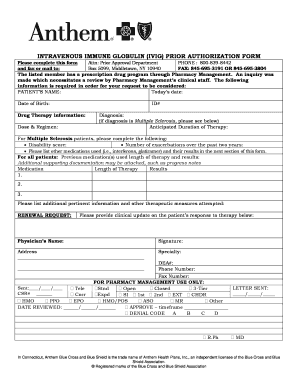
If you do not obtain prior approval there may be a reduction or denial of your benefit. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan.
Https Www11 Anthem Com Ca Provider F1 S0 T0 Pw E229275 Pdf Refer Provider
You will be notified by fax if the request is approved.

Anthem blue cross prior authorization form. Requests will be confidentially reviewed according to payment criteria developed by Blue Cross in consultation with independent health care consultants. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Provider Forms Guides At Anthem were committed to providing you with the tools you need to deliver quality care to our members.
To find a prior authorization form visit our forms page or click on the links below. Easily find and download forms guides and other related documentation that you need to do business with Anthem all in one convenient location. The Blue Cross and Blue Shield Association.
Medicaid only BCCHP and MMAI Medicaid Service Authorization Dispute Resolution Request Form. Anthem Blue Cross is the trade name of Blue Cross of California. Anthem Blue Cross is the trade name of Blue Cross of California and Anthem Blue Cross Partnership Plan is the trade name of Blue Cross of California Partnership Plan Inc.
Our Interactive Care Reviewer ICR tool via Availity is the preferred method for submitting prior authorization requests offering a streamlined and efficient experience for providers requesting inpatient and outpatient medical or behavioral health services for our. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Certain medical services and treatments need approval before you receive care.
Prior coverage for PPO and dental plans only Attach additional sheets if necessary. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. Anthem Blue Cross Enrollment Form 1 Purpose.
Medicaid only BCCHP and MMAI. Important for the review eg. Not getting prior authorization beforehand can result in a payment penalty for you or the member.
Form Title Networks Expedited Pre-service Clinical Appeal Form. Information contained in this form is Protected Health Information under HIPAA. These standard forms can be used across payers and health benefit managers.
Blue Cross and Blue Shield Association. Select the Drug List Search tab to access up-to-date coverage information in your drug list including details about brands and generics dosagestrength options and information about prior authorization of your drug. You can also submit your request online through Availity.
Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required. During this time you can still find all forms and guides on our legacy site. The Blue Cross name and symbol are registered marks of the Blue Cross Association.
Provider Forms Guides. Anthem Blue Cross and Anthem Blue Cross Life and Health Insurance Company are independent licensees of the Blue Cross Association. Fax completed forms to FutureScripts at 1-888-671-5285 for review.
In some cases additional. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. ANTHEM is a registered trademark of Anthem Insurance Companies Inc.
Chart notes or lab data to support the prior authorization or step-therapy exception request. Use one form per member. ANVPEC-1497-20 December 2020 Please check the appropriate box below and send only the corresponding authorization type to that fax number.
Independent licensees of the Blue Cross Association. Medicaid Claims Inquiry or Dispute Request Form. We review them to ensure they are medically necessary.
ANTHEM is a registered trademark of Anthem Insurance Companies Inc. When completing a prior authorization form be sure to supply all requested information. We are currently in the process of enhancing this forms library.
Requests for the following services can be made by fax or mail. A standardized or uniform prior authorization PA form may be required in certain states to submit PA requests to a health plan for review along with the necessary clinical documentation. This is called prior approval precertification or preauthorization.
Anthem is a registered trademark of Anthem Insurance Companies Inc. Submit a prior authorization Reviewed by BlueCross BlueShield. AWIPEC-0649-18 January 2018 Prior Authorization Form for Medical Injectables If the following information is not complete correct andor legible the prior authorization PA process can be delayed.
For a service requiring a pre-service review there isnt a penalty but Premera will hold the claim and ask for medical records Note. Prior authorizations cant be submitted by phone. Anthem Blue Cross Anthem is available by fax or Interactive Care Reviewer ICR 247 to accept prior authorization requests.
Prior Authorization is a pre-approval process to determine if certain prescription drugs will be reimbursed under a members benefit plan. Please fill out the Prescription Drug Prior Authorization Or Step Therapy Exception Request Form and fax it to 877 327-8009. On this page you can easily find and download forms and guides with the information you need to support both patients and your staff.
Premera requires prior authorization for many services before they take place. Make sure you include your office telephone and fax numbers.
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
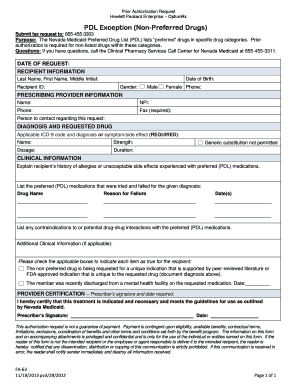 2012 Form Nv Fa 63 Fill Online Printable Fillable Blank Pdffiller
2012 Form Nv Fa 63 Fill Online Printable Fillable Blank Pdffiller
 Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Https Www Anthem Com Provider Noapplication F0 S0 T0 Pw E228625 Pdf Na Pharminfo
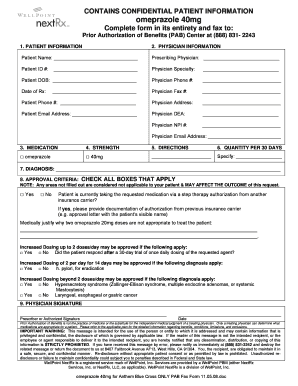
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Https Www Empireblue Com Provider Noapplication F3 S2 T2 Pw Ad067834 Pdf Refer Ehpprovider
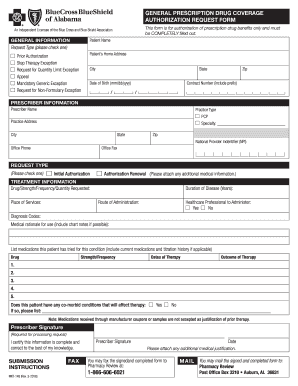 Blue Cross Blue Shield Of Alabama Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Blue Cross Blue Shield Of Alabama Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
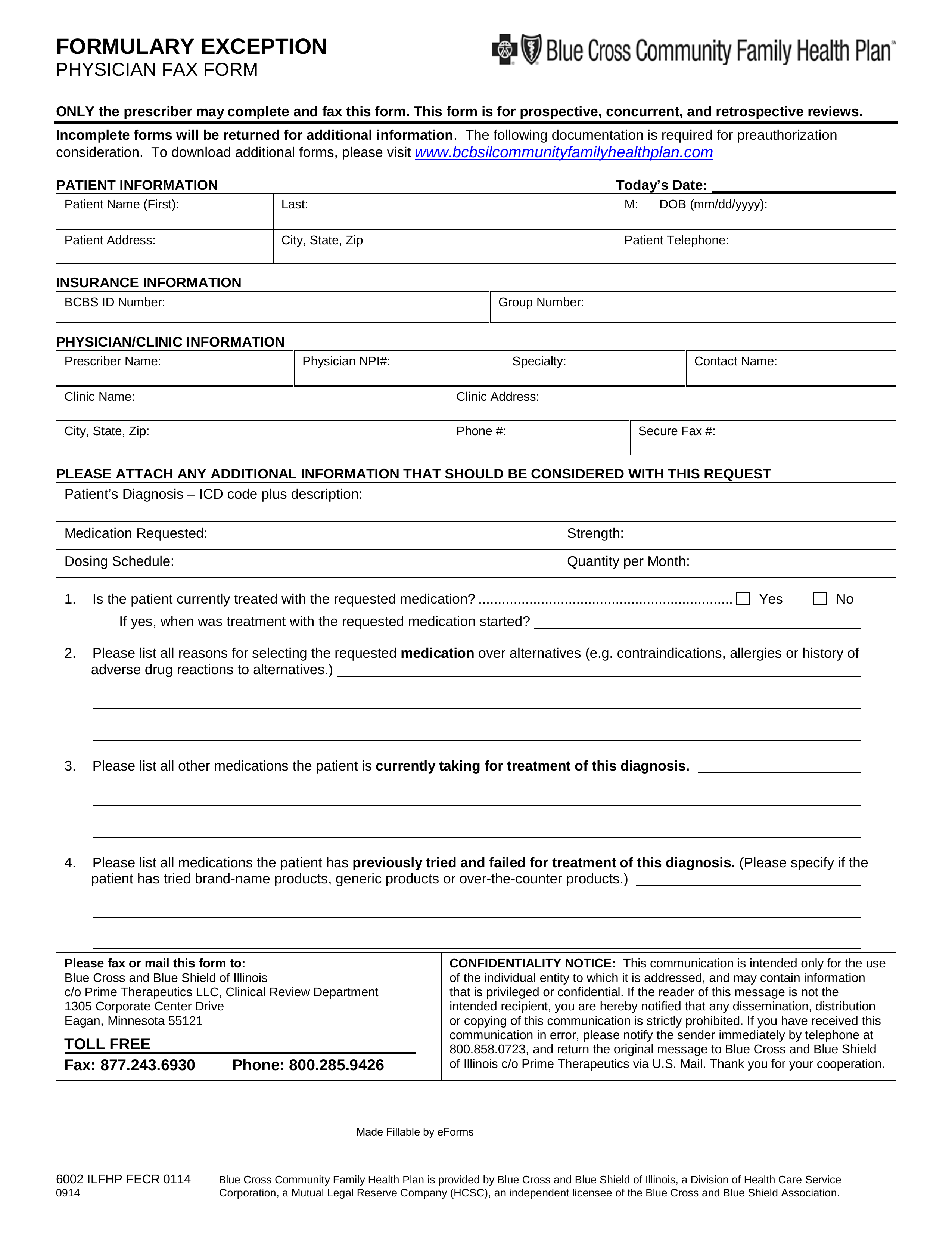 Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
Https Www Bcbsil Com Pdf Education Forms Fhp Preauth Form Pdf
 Fillable Online Anthem Prior Auth Request For Form Fax Email Print Pdffiller
Fillable Online Anthem Prior Auth Request For Form Fax Email Print Pdffiller
 Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
 Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Https Bluecrossnc Com Sites Default Files Document Attachment Common Pdfs Hmo Ppo General Quantity Limitations Fax Request Form Pdf
 Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.