An estimated 663000 Covered California enrollees who currently receive federal financial help. Coverage is expected to get more expensive with nationwide costs expected to rise 55 percent every year between now and 2026 and Obamacare premiums in California projected to increase 35 percent by 2021 according to Covered California.
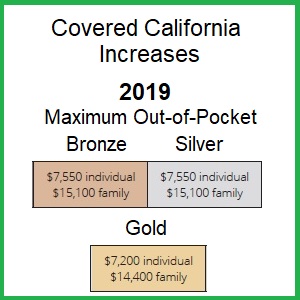 Maximum Out Of Pocket Amount Jumps 7 For 2019 Covered California Plans
Maximum Out Of Pocket Amount Jumps 7 For 2019 Covered California Plans
The high cost of health care was ranked as Americans top financial concern in a Gallup poll last year.

Covered california expensive. Federal ACA subsidies through Covered California have made coverage more affordable for hundreds of thousands of Californians. The law goes into effect in January and will cost families as much as 2100 per year if they go without insurance. Newsoms approval expands subsidies for people who purchase health insurance on the states Covered California exchange.
A recent budget deal approved by the state legislature is expected to ease some of health care expenses burden on low and moderate-income families. For many individuals and families 2018 is the year of extreme sticker shock over the rates for health insurance. Bronze 60 California coverage maximum out of pocket maximum of 8200 for 2021.
Covered California officials said. Covered California the health insurance exchange that is supposed to be protecting people from predatory health insurance premiums. Well first of all its California so virtually everything is more expensive than most of the rest of the USA.
The best way to get a quick estimate of the price you would pay is to use the Shop and Compare Tool. Tuesday I call Covered California no one can explain the. Those in the 400-600 range of FPL who are over 50 years of age and those who live in areas where health insurance premiums are more expensive are more likely to receive state subsidies.
The budget which is still awaiting Gov. 201505 So because Covered California couldnt handle my address change when I became eligible for Medi-Cal see above it turns out that my Medi-Cal got completely screwed up its unclear who is completely at fault here between Medi-Cal and Covered California. An estimated 23000 Covered California enrollees whose annual household income.
Non-standard off-exchange health plans are usually less expensive than the Covered California designed plans. On April 30th I paid 58700 for medical and 10300 dental. Platinum These plans cover 90 percent of the actuarial value of the costs and health expenses.
Its the only place where you can get financial help when you buy. Covered California can be priced much lower and you can change plans. Very few health care services are subject to the medical deductible of 4000.
This means you pay full cost for all your medical services until or if you meet the deductible. Again our services as Certified Covered California agents is free to you. Double Digits Over the last two years Covered California has managed to stem the increasing cost of plans to the tune of single-digit percentages.
Older Californians Struggle to Afford Lowest-Cost Plans on Covered California May 14 2018 Under the Affordable Care Act ACA California has now covered 93 of our adult population a record high. They will be eligible to receive an average of an additional 15 per household per month which will help them save an average of 5 percent on their current premiums. They will always be the most expensive plans on the Covered California calucator.
To bring us up to date Ive been receiving letters from Southern California my new address about my. Silver 70 on the other hand has most health care service at a set copayment or 20 coinsurance. Premiums tend to be higher in Northern California and in areas like Monterey County.
Covered California is a free service from the state of California that connects Californians with brand-name health insurance under the Patient Protection and Affordable Care Act. Second Covered California is just your states version of ObamaCare which has managed to more than double the cost of individual health insurance premiums since 2014. The price is based on your estimated income for the coverage year your ZIP code your household size and your age.
The cost of health insurance varies. Monday night late I sign on to the website and my premium for medical jumped to the same as my Cobra 116600 a month. This plan has a 8150 individual deductible and 16300 on a family basis.
The out of pocket maximum is 8150 for an individual and 16300 for a family. Cobra is really expensive and you might not be able to change plans. The same couple in 2020 would be eligible for 1310 in monthly state subsidies or nearly 16000 per year and the lowest cost Silver plan.
If you qualify for a Covered Ca tax credit its hard to justify paying full premium for Cobra. Today Covered California announced regrettable news indicating that they were unable to stem the tide of rising costs indicating that premiums will be 132 more expensive in 2017. If you are a low- or moderate-income Californian you may get help buying insurance from Covered California through.