Contrastingly this is where Talkspace has a significant benefit over BetterHelp. Verifying coverage of virtual services to replace in-person visits and telehealth benefits Verifying coverage of virtual services to replace in-person visits and telehealth benefits.
 Is Betterhelp Covered By Insurance And Other Answers
Is Betterhelp Covered By Insurance And Other Answers
Cigna Humana Premera Blue Cross Blue Shield and Optum all can help cut off a portion of the heavy Talkspace treatment expense.
:max_bytes(150000):strip_icc()/betterhep-c24a5fed18fa46c0814fb6e8da1297c0.jpg)
Betterhelp blue cross blue shield. BetterHelp may be right for you if youre looking to improve the quality of your life. BetterHelp is a subscription service that provides users with access to online therapy. We also have counselors who are specialized in specific issues such as stress anxiety relationships parenting depression addictions eating sleeping trauma.
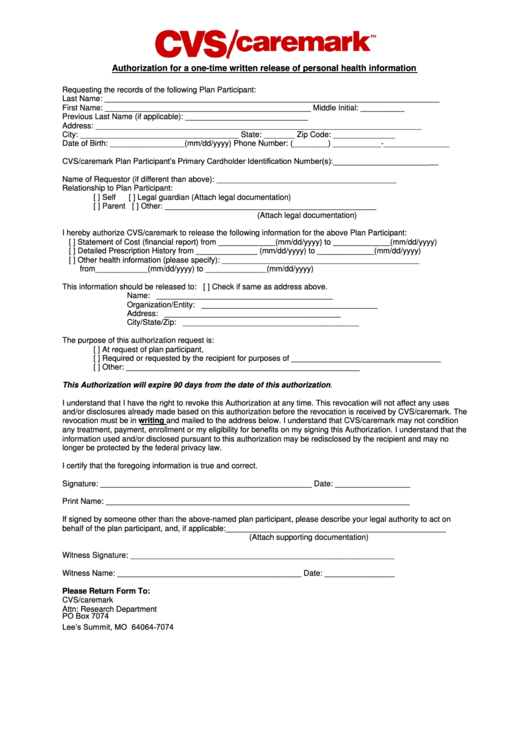
Thats why they provide affordable discreet and convenient access to their licensed therapists. Does Blue Cross Blue Shield Cover Betterhelp. Even though Blue Cross Blue Shield is one of the insurance providers that cover both in-office therapy and online therapy in their plans insurance providers require the therapist to send an official diagnosis for you to apply for the coverage.
Read more about it here. BetterHelps Terms of Service do not authorize counselors to provide a medical diagnosis to users. One of the largest and leading online-based counseling platforms is the BetterHelp.
We have a variety of great therapists to choose from. Currently Talkspace is covered by the nations biggest health insurers including Cigna Optum Premera Blue Cross Blue Shield and Humana. The result of this rigorous 4-5 week process is that only about 15 of the therapists who apply to work through BetterHelp are.
Generally MHPAEA requires that certain group and. Although Blue Cross Blue Shield BCBS recognizes telemental health and provides coverage for such services the online mental health platform discourages the use of insurance for. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States.
Cigna Humana and other major insurers will cover costs of Talkspace. You can also see how Dr. Find BlueCross and BlueShield Therapists Psychologists and BlueCross and BlueShield Counseling in Savannah Chatham County Georgia get help for BlueCross and BlueShield in Savannah get help.
In the United States Puerto Rico and US. So if you have very good health insurance from Cigna Humana Premera Blue Cross Blue Shield or Optum you might be able to shave off some of the extra cost of Talkspace as compared to BetterHelp cost. The organization works many ways to face the challenges of human lives.
Oleshansky you can easily book an appointment with her online. Talkspace might actually be covered by the insurance of around 40 million Americans at this moment. According to the final rules MHPAEA applies to certain group and individual health plans with plan years or in the individual market policy years on or after July 1 2014.
Outside the United States. Excellus BlueCross BlueShield an independent licensee of the Blue Cross Blue Shield Association is a nonprofit health plan with 15 million upstate New York members. Blue Cross Blue Shield members can search for doctors hospitals and dentists.
BetterHelp is convenient and secure as well. No other national carrier covers as many workers and retirees along with families as the Blue. For insurance coverage she accepts Blue Cross Blue Shield of Michigan and Medicare.
Oleshansky has been practicing for over 17 years since getting her license to practice in Michigan. In 2008 Congress passed the Mental Health Parity and Addiction Equity Act of 2008 MHPAEA. BetterHelp services are generally not covered by health insurance Medicare or Medicaid.
In addition to checking credentials each potential provider needs to complete a case study exam by a licensed clinician and a be evaluated in a video interview. We encourage you to do your research on financing therapy and we hope that BetterHelp is part of your research. You can talk to a psychologist a clinical social worker a marriage and family therapist or.
We then cross-check their licensure information with their respective state licensing board. If you want to see Dr. Whenever there is anything that interferes with your happiness or prevents you from achieving your goals we may be able to help.
She is currently working at Talkspace Online Counseling to provide care. Blue Cross Blue Shield plans also cover more than 50 percent of state government employees and retirees as well as their families via the Federal Employees ProgramThe program which was created following the enactment of the Federal Employees Health Benefits Act has about 56million members 1. The Blue Cross Blue Shield Association is an.
The companys mission is to help people live healthier and more secure lives through access to high-quality affordable health care. It is completely anonymous if you wish and can be accessed from the privacy of your home.