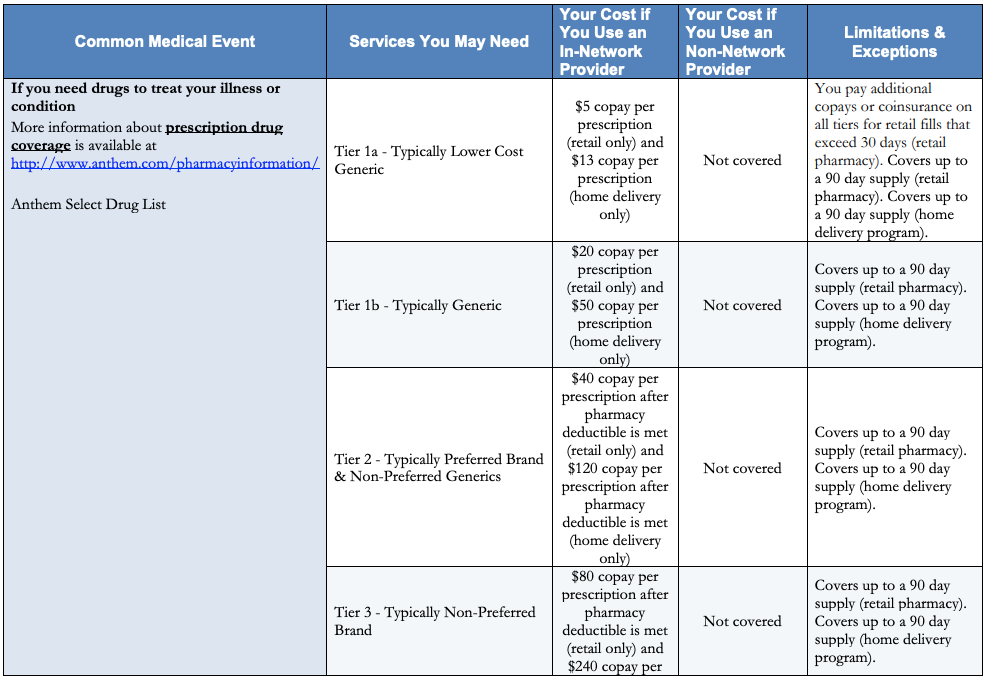
You may save money by using lower tier drugs. You can ask us to waive coverage restrictions or limits on your drug.
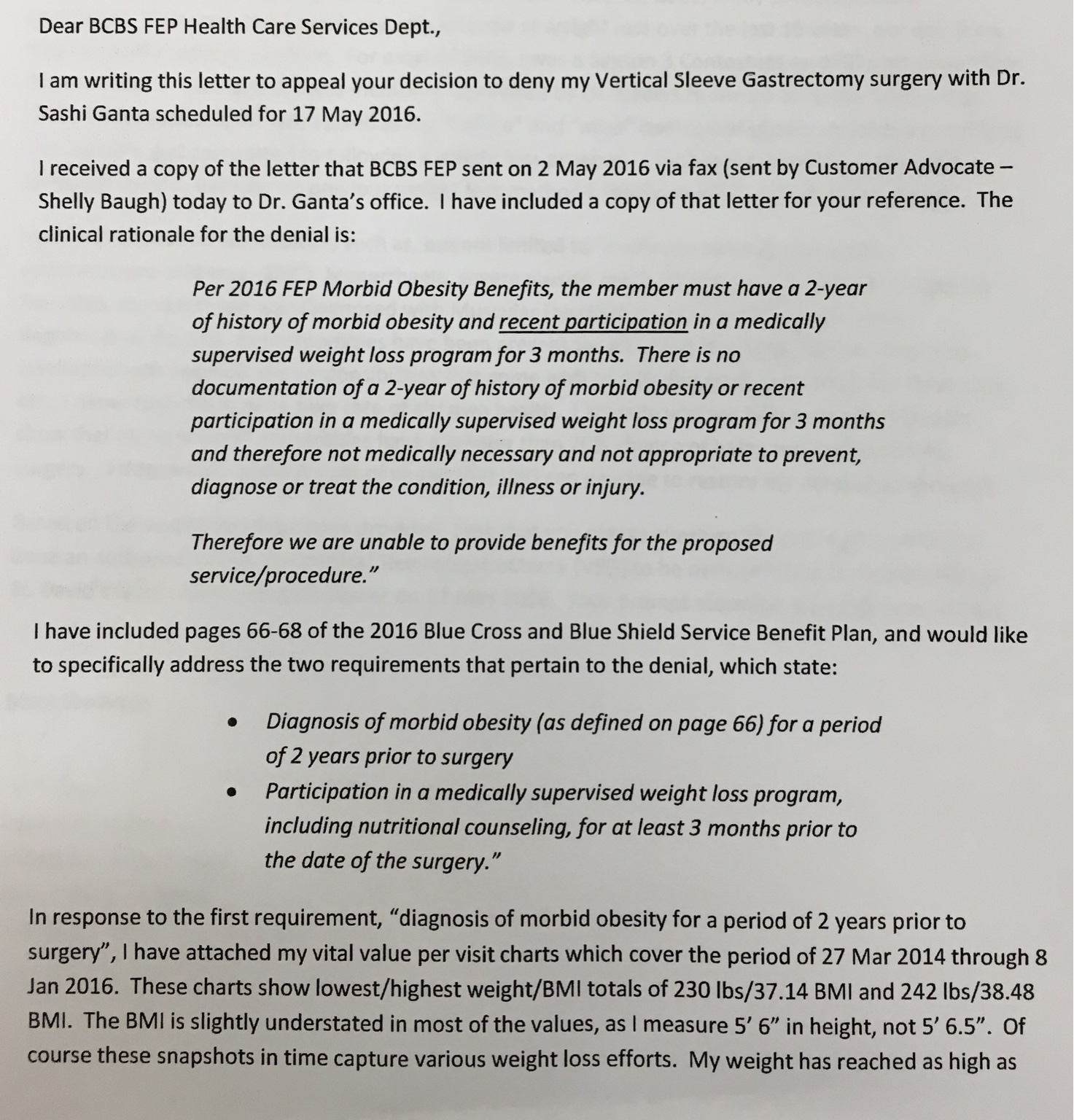
 What Is A Summary Of Benefits And Coverage And How Should I Use It Goodrx
What Is A Summary Of Benefits And Coverage And How Should I Use It Goodrx
These can include drugs that must be given to you by a health care provider.
Anthem blue cross medication coverage. Andor Empire HealthChoice Assurance Inc licensees of the Blue Cross and Blue Shield Association an association of independent Blue Cross and Blue Shield Plans serving residents and businesses in the 28 eastern and southeastern counties of New York State. For example drugs used for cosmetic purposes usually are not covered. You can ask us to cover a formulary drug at a lower cost-sharing level.
Anthem Blue Cross and Blue Shield Drug List Your prescription drug benefit includes coverage for medications that youll find on the Anthem Preferred Drug List. Orth-Evra patch and Nuvaring will be covered at 100 with no member copayment. Or you can get drug coverage through our Medicare Advantage plans.
Formerly known as Kapidex Covered PPI medications omeprazole generic Prilosec lansoprazole generic. If approved this would lower the amount you must pay for your drug. 210 minimum for a 31 to 90-day supply.
Drug List To be used by members who have a three 3 tiered drug plan. You can also buy a Medicare Part D plan to complement a Medicare Supplement plan. What if my medication is not listed.
We have two drug lists that show which drugs are in your plan. American Addiction Centers AAC is in-network with many insurance companies including Anthem at some of our facilities. Combined amount plus your deductible You will be in the coverage gap.
Set coverage level Finally the Pt committee discussed this information decided which medications should be included on the drug listformulary and set coverage levels. Services provided by Empire HealthChoice HMO Inc. Anthem Blue Cross drug and alcohol rehab coverage does typically cover drug and alcohol rehab but the extent of coverage highly depends upon the particular patient and their insurance plan as well as the provider at hand.
Anthem also covers many over-the-counter OTC medicines with a prescription from your doctor. What is a Drug List. Your request should include why a specific drug is needed and how much is needed.
Your Medicare prescription drug coverage as a member of Anthem Blue MedicareRx Premier PDP This booklet gives you the details about your Medicare prescription drug coverage from January 1 December 31 2018. If your drug has a quantity limit you can ask. Tier 4 Preferred specialty.
This is known as prior authorization PA. AKA donut hole You will be required to pay 25 for prescription drugs unless your plan offers additional coverage. Examples of these drugs are contraceptive implants and chemo infusion.
Anthem Blue Cross and Blue Shield Anthem prescription drug benefits include medications on the Anthem Preferred Drug List. For example for certain drugs our plan limits the amount of the drug that we will cover. Anthem Blue Cross Cal MediConnect Plan Medicare-Medicaid Plan is a health plan that contracts with both Medicare and Medi-Cal to provide benefits of both programs to enrollees.
Please keep it in a safe place. This drug list contains the most commonly prescribed drugs and their associated tier. Plus you have access to up-to-date coverage information in your drug list including details about brands and generics dosagestrength options and information about prior authorization of your drug.
If you are taking or prescribed a drug that is not on your plans Drug List call the number on your member ID card to see if the drug may be covered. There are often different ways to get coverage for prescription drugs. Tier 5 Non-preferred specialty.
Anthem Blue Cross Gap Coverage In 2021 once you and your plan provider have spent 4130 on covered drugs. Anthem Blue Cross is the trade name for Blue Cross of California. This is an important legal document.
You can buy prescription drug coverage alone as a Medicare Part D plan. If youre not sure whether these lists apply to your plan check with your employer or call the Customer Support number printed on your ID card. You may need to get approval from us for certain drugs.
These drugs are often given to you in a hospital doctors office or health care setting. The Anthem Blue Cross and Blue Shield Healthcare Solutions Anthem PDL includes all medicines covered by Medicaid. Or go to.
Anthem Blue Cross Blue Shield prescription drug benefits include medications available on the Anthem Drug List. Tier 3 Non-preferred brand. You can save money when your doctor prescribes medications on the drug list.
Some drugs are covered under your medical plan instead of your pharmacy benefits. Preferred Drug List PDL The Preferred Drug List PDL has the medicines your plan pays for as long as you have a prescription. Our prescription drug benefits can offer potential savings when your physician prescribes medications on the drug list.
This means theyre also more affordable for you. Your benefits include a wide range of prescription drugs. 60 of our allowance 75 minimum for up to a 30-day supply.
It explains how to get coverage for the prescription drugs you need. Anthem Blue Cross and Blue Cross of California Partnership Plan. When your doctor prescribes a drug youve never taken before you may wonder if your plan will help pay for it.
If your drug is not listed please call Anthem Member Services at. Tier 4 and 5 specialty drugs are limited to a. The Anthem Preferred Drug List also called a formulary has drugs on it that are approved by the US.
Your coverage has limitations and exclusions. Blue Cross Blue Shield of Michigan and Blue Care Network members under age 65 with prescription drug coverage.




/best-dental-insurance-providers-4169737_final2-a801550ef6a64ef99aed716a2503078b.png)
/cigna-logo-wallpaper-e1474921230453-fa540a75903245a18ff0e794e1e1f7ec.jpg)