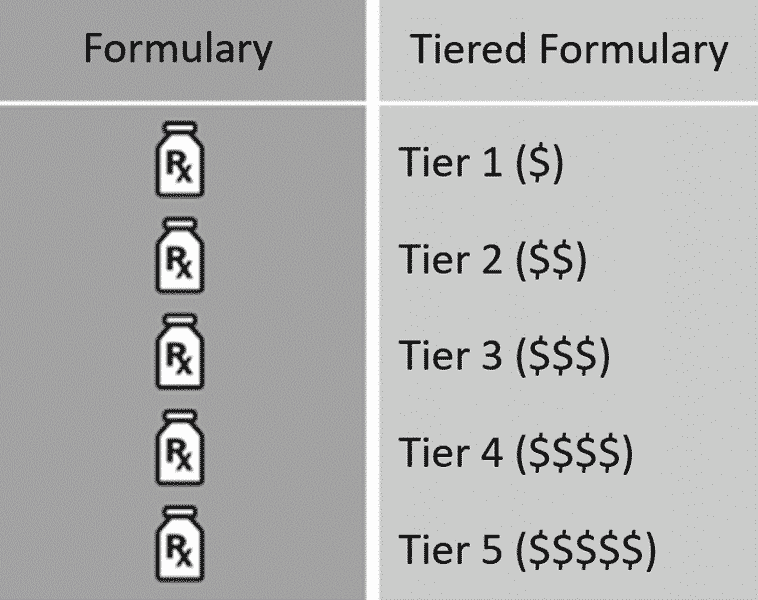
For the most recent list of excluded drugs read our Custom and Clinical Drug List Exclusions PDF. A formulary is a list of covered drugs selected by our plan in consultation with a team of health care providers which represents the prescription therapies believed to be a necessary part of a quality treatment program.
 2013 Formulary Empire Blue Cross Blue Shield
2013 Formulary Empire Blue Cross Blue Shield
Sections of this page.
Blue cross blue shield formulary. When it refers to plan or our plan it means Medicare Plus Blue Group PPO or Prescription Blue Group PDP. If you are a member with Empire BlueCross BlueShields pharmacy coverage click on the link below to log in and automatically connect to the drug list that applies to your pharmacy benefits. In all cases a doctor is expected to select the most appropriate drug therapy for their patient.
Blue Cross Blue Shield of Massachusetts Medicare Advantage Plans cover both brand name drugs and generic drugs. A formulary is a list of covered drugs selected by Medicare PPO Blue SaverRx Medicare HMO Blue SaverRx HMO Medicare PPO Blue ValueRx PPO Medicare HMO Blue ValueRx HMO in consultation with a team of health care providers which represents the prescription therapies believed to be a necessary part of a quality treatment program. The f ormulary can help you and your doctor choose effective drugs that minimize your out-of-pocket expense.
IntroductIon BlueCross Blue Shield of Western New York has established an independent committee of practicing physicians. Please review this document to make sure that it still contains the drugs you take. When this drug list formulary refers to we us or our it means Blue Cross Blue Shield.
Our plan will generally cover the drugs listed in our formulary as long as the drug is. Generic drugs have the same active ingredient formula as a brand name drug. The drugs listed will be covered as long as you.
You can also learn more about some of our online tools like pricing a. Blue Cross Blue Shield of Arizonas Prescription Medication Formulary for EverydayHealth TrueHealth and AdvanceHealth Effective 1120 Your prescription medications fall into one of six categories or tiers Each tier has different copay or out of pocket expense. Familiarize yourself with the specifics of your plans formulary.
See how we help keep your out-of-pocket costs low for the medications you and your family need. The Blue Cross and Blue Shield of Illinois BCBSIL Prescription Drug List also known as a Formulary is designed to serve as a reference guide to pharmaceutical products. Select Blue Cross Blue Shield Global or GeoBlue if you have international.
The formulary is a list of your covered prescription drugs. The drugs on this list are not covered on the commercial Blue Cross Blue Shield Custom and Clinical drug lists. The formulary is a list of our covered prescription drugs including generic brand name and specialty drugs.
The preferred alternatives on this list have similar effectiveness quality and safety but at a fraction of the cost. The BlueCross BlueShield of Western New York Formulary 1 is a list of drugs to help guide physicians and pharmacists to select the medication that provides the appropriate treatment for the best price. This document includes a list of the drugs formulary for our plan which is current as of May 1 2021.
The drug list sometimes called a formulary is a list showing the drugs that can be covered by the plan. However the drug list is not intended to be a substitute for a doctors clinical knowledge and judgment. Blue Cross Blue Shield of Massachusetts is an Independent Licensee of the Blue Cross and Blue Shield Association.
In the United States Puerto Rico and US. 2020 Basic Option Formulary. Formulary which offers drug treatment choices for covered medical conditions.
Medications are categorized by tier based on their quality. 2020 Standard Option Formulary. Outside the United States.
This formulary has changed since last year. The BlueCross BlueShield Medicaid Formulary Guide is a list of drugs to help guide physicians and phar-macists to select the medication that provides the appropriate treatment for the best price. IntroductIon BlueCross Blue Shield of Western New York has established an independent committee of practicing physicians.
Food and Drug Administration and. Blue Cross Blue Shield members can search for doctors hospitals and dentists. Generic drugs usually cost less than brand name drugs and are rated by the Food and Drug Administration FDA to be as safe and effective as brand name drugs.
Have a medical need for them Fill the medication orders at an in-network pharmacy. What is the Blue Cross Community Health Plans the Plan drug list. Blue Cross Blue Shield of Michigan and Blue Care Networks Custom Drug List is a useful reference and educational tool for prescribers pharmacists and members.
You can buy formulary drugs at participating retail mail-order and specialty pharmacies. It includes generic brand name and specialty drugs as well as Preferred drugs that when selected will lower your out-of-pocket costs. We regularly update this list with medications approved by the US.
2020 FEP Blue Focus Formulary. Press alt to open this menu. When this drug list formulary refers to we us or our it means Blue Cross Blue Shield of Michigan.
The formulary is a list of prescription drugs covered on your plan. Note to existing members. See more of Blue Cross and Blue Shield Federal Employee Program on Facebook.
For an updated formulary please contact us.