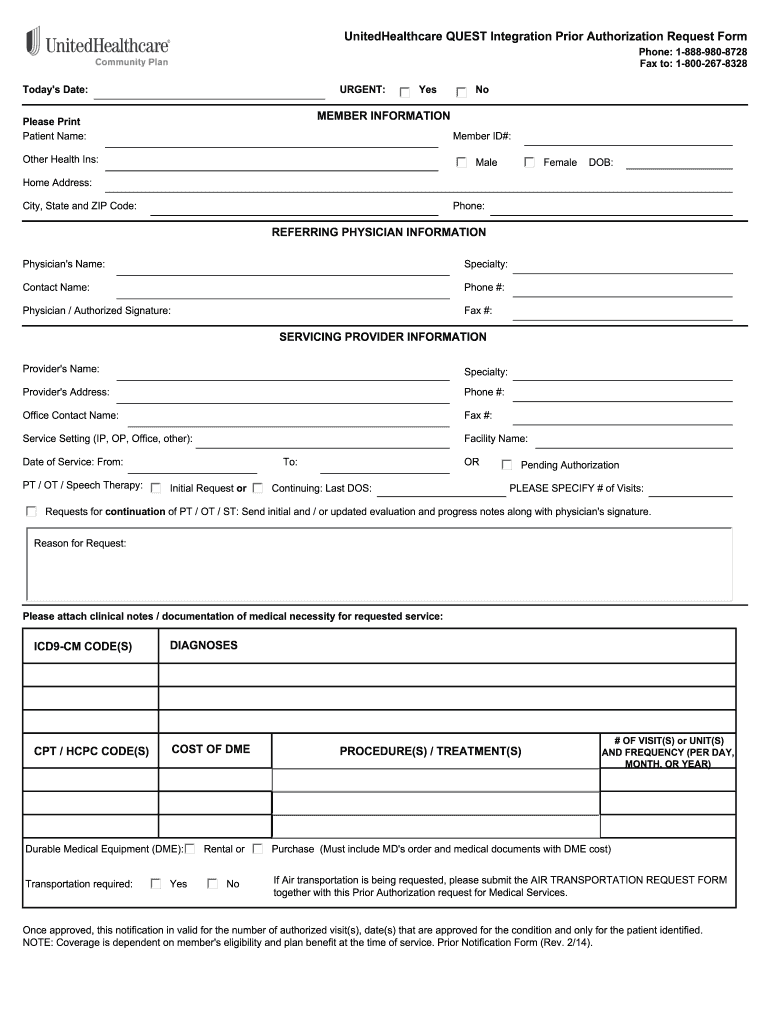
In general your network primary physician and other in-network providers are responsible for obtaining prior authorization before they provide these services to you. Standalone authorization form pdf Standalone personal representative form pdf These optional forms are used by the member to provide UnitedHealthcare with authorization to discuss their claim with someone other than the member.
 United Healthcare Authorization Forms Fill Online Printable Fillable Blank Pdffiller
United Healthcare Authorization Forms Fill Online Printable Fillable Blank Pdffiller
Accident Protection Plan Claim Form Packet pdf Standalone authorization.
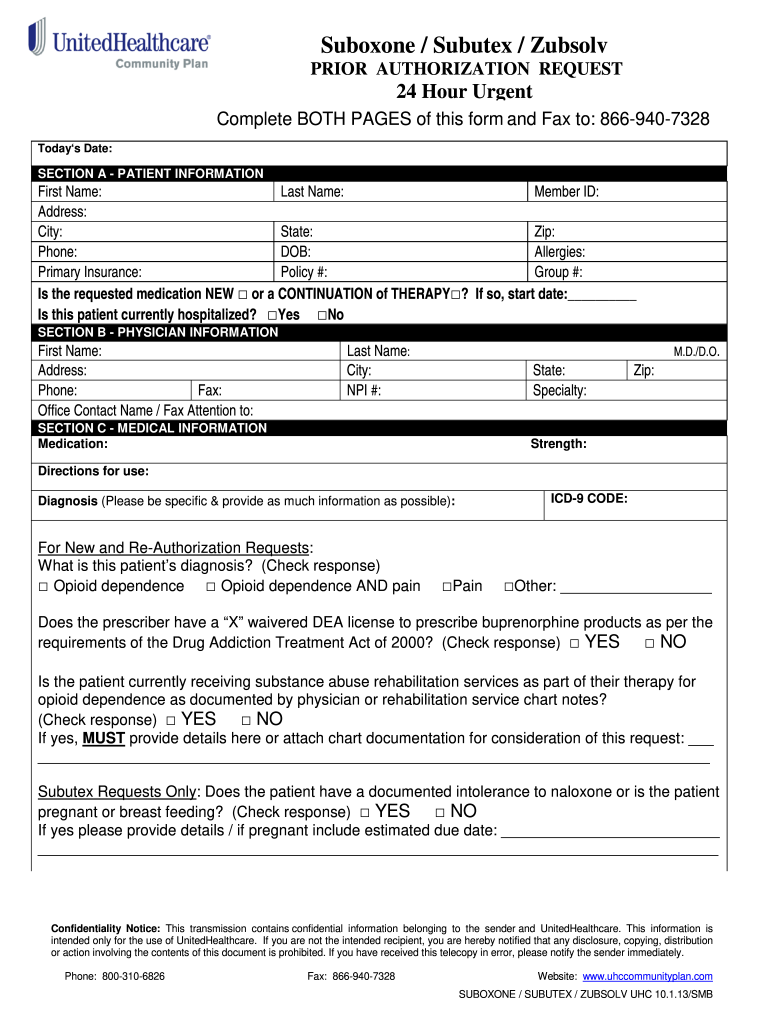
United prior authorization. If a prior authorization is denied you may be responsible for the cost of. Advance NotificationPrior Authorization Effective January 1 2016 General Information This list outlines the prior authorization requirements inpatient and outpatient for UnitedHealthcare Community Plan in Louisiana. Check the status or update a previously submitted request for prior authorization or notification using the reference number or member or provider information.
2019 United HealthCare Services Inc. The Prior Authorization PA unit at AHCCCS authorizes specific services prior to delivery of medical related services. One way for healthcare professionals and their staff to tackle the complicated prior authorization landscape is to pursue a certification as a Prior Authorization Certified Specialist PACS offered by the National Board of Prior Authorization Specialists NBPAS.
Provider may complete a Face-To-Face assessment via telehealth. Without this prior approval your health insurance provider may not pay for your medication or operation leaving you with the bill instead. Please use this chart to request prior authorization before providing services to our members in the following.
Upload clinical notes or attach medical records and images to a request. Your doctor is responsible for getting a prior authorization. Step 1 Enter todays date at the top of the page.
Step 2 Section A must be completed with. Standard Prior Authorization Request Form Please submit your request online using our Prior Authorization and Notification tool on Link. Form can be faxed to.
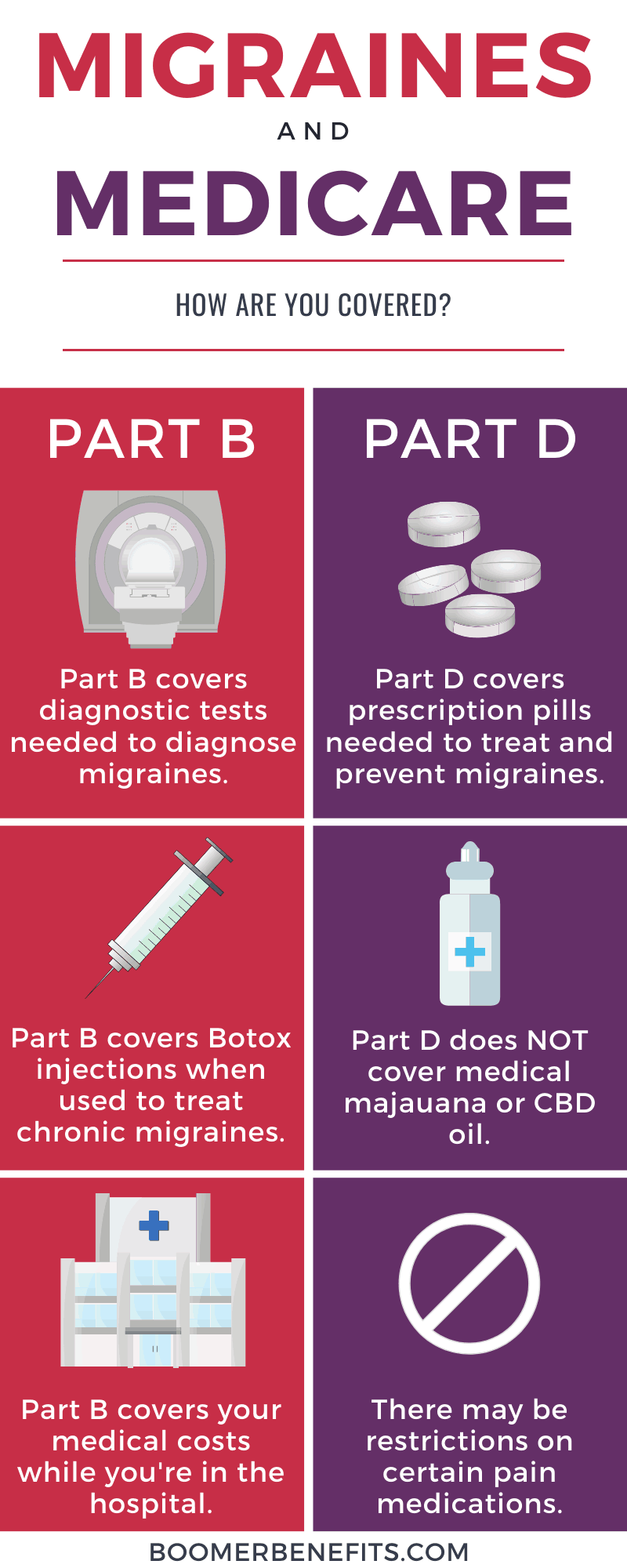
You may also initiate your request by phone by calling the number on the back of the members health plan ID card. For prior authorizations for services that were completed before Oct. Prior authorization is a requirement that your physician obtains approval from your healthcare provider before prescribing a specific medication for you or to performing a particular operation.
UnitedHealthcare requires prior authorization for certain covered health services. Then select the Prior Authorization and Notification app tile on your Link dashboard. The purpose of this form is to demonstrate medical justification for.
BHRF Admission Notification Form. ADMINISTRATIVE 24554 Effective Date. Supervisor - Prior Authorization Intake - Phoenix AZ UnitedHealth Group 37 Phoenix AZ 85002 Central City area The Supervisor of Prior Authorization Intake will be responsible for managing a team of front line intake coordinators on our Prior Authorization team.
2021 Mar 24S0264-410X 2100315-7. There are some benefits however for which you are responsible for obtaining prior authorization as indicated in this SPD. If a prior authorization is approved those services will be covered by your health plan.
Maryland Michigan Missouri New. COVID-19 vaccination attitudes values and intentions among United States adults prior to emergency use authorization. Read the job description for Prior Authorization RN - Telecommute in Nashville TN US.
Use the Prior Authorization and Notification app on Link. Forms used in PA Unit include the following. For prior authorizations for services that were completed on Oct.
This is called prior authorization. UnitedHealthcare Prior Rx Authorization Form UnitedHealthcare prior authorization form. Your primary UnitedHealthcare prior authorization resource the Prior Authorization and Notification tool is available on Link UnitedHealthcares self-service tools.
They will provide us with the information needed. UnitedHealthcare requires that care providers complete the notificationprior authorization process for genetic and molecular testing performed in an outpatient setting for UnitedHealthcare Community Plan members in these states. PA request status can be viewed online.
Apply to Clinical Pharmacist Prior Authorization Specialist Pharmacist and more. Submit a new request for medical prior authorization or to notify UnitedHealthcare of an inpatient admission. 1 2019 a new prior authorization is required.
Online ahead of print. May 1 2018 INSTRUCTIONS FOR USE. To request prior authorization please submit your request online or by phone or fax.
Services Requiring Prior Authorization Page 1 of 18 UnitedHealthcare Oxford Administrative Policy Effective 05012018 1996-2018 Oxford Health Plans LLC SERVICES REQUIRING PRIOR AUTHORIZATION Policy Number. 1 2019 or later UnitedHealthcare is extending prior authorizations through Sept.