When Does Medicare Supplement Open Enrollment Occur. Rules about when you can make changes and the type of changes you can make are different.
 Medicare Enrollment Periods What You Need To Know Aetna Medicare
Medicare Enrollment Periods What You Need To Know Aetna Medicare
After this enrollment period you may not be able to buy a Medigap policy.
Medicare supplement enrollment. You must meet both qualifications to be eligible for Medigaps open enrollment period. These chances to make changes are called Special Enrollment Periods SEPs. Shop 2020 Medicare plans.
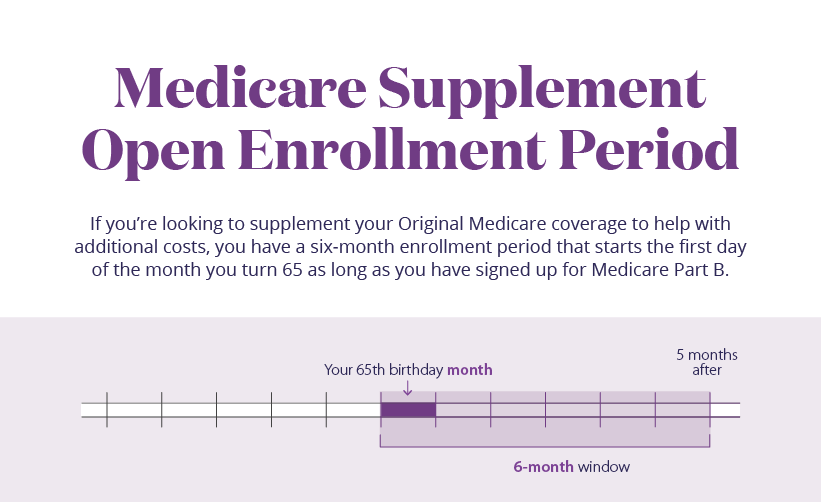
Your Medicare Supplement Open Enrollment Period is a once in a lifetime window that allows you to enroll in any Medigap plan without answering health questions. Annons You must order now to get Meticore and secure your order while stocks last. Annons You must order now to get Meticore and secure your order while stocks last.
Special Enrollment Periods In some cases you might be able to enroll in Medicare or get other Medicare coverage outside of the regular enrollment periods. 65 years old and. Insurance companies cannot deny you Medigap coverage or charge you a higher fee for pre-existing health conditions if.
Unlike the Medicare OEP that happens once every year you have only one Medigap OEP. A Medicare Supplement Special Enrollment Period restores your ability to enroll in Medicare Supplement. Medicare coverage is a vital part of health and wellness for many individuals as it includes coverage for healthcare expenses for a wide.
Medicare Supplement Insurance Medigap Enrollment Your Medigap Open Enrollment Period starts as soon as you are age 65 or older and are enrolled in Medicare Part B. You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life like if you move or you lose other insurance coverage. Throughout this period you can enroll in any Medigap plan offered in your service area with guaranteed issue.
Your open enrollment period begins when you are both. Medicare Supplement Open Enrollment Period. This is the six-month period that starts on first day of the month that you are both 65 or older and enrolled in Medicare Part B.
This period automatically starts the month youre 65 and enrolled in Medicare Part B Medical Insurance and it cant be changed or repeated. Open Enrollment Period for additional Medicare insurance coverage Medicare Open Enrollment Period begins the first day of the month in which you are at least 65 and covered under Medicare Part B. Medicare Supplement Enrollment Periods When you are first eligible for Medicare you can enroll in a Medigap plan.
There are many ways to qualify for special enrollment. Dont Buy Meticore Unless Youve Seen This Massive Discount Exclusive Bonuses. Protect the best years ahead.
For example Medigap Open Enrollment can start when you turn 65 or first become eligible for Medicare. Annons Find your best rate from over 4700 Medicare plans nationwide. A Medicare Supplement Special Enrollment Period restores your ability to enroll in Medicare Supplement Medigap at fair prices even if your Medigap Open Enrollment Period is over.
Protect the best years ahead. Please note that this table doesnt include every situation that might qualify you for a Special Enrollment Period. In general the best time to enroll in a Medicare Supplement insurance plan is during your Medigap Open Enrollment Period.
For traditional Medigap customers the Medicare supplement open enrollment period lasts for six months. If youre able to buy one it may cost more due to past or present health problems. Shop 2020 Medicare plans.
Enrolled in Medicare Part B. When can I enroll in a Medicare Supplement Plan. When newly eligible for Medicare you enter a seven-month Initial Enrollment Period IEP which begins three months before your 65th birthday and ends three months after the month of your birthday.
Medicare Supplement Insurance Medigap has a six-month open enrollment period OEP. Open enrollment for Medigap also known as Medicare supplement insurance is the 6-month period that begins the month you turn 65 years old. This Medigap Open Enrollment Period starts after you enrolled in Medicare Part B.
This window begins the month you turn 65 and enroll in Medicare Part B. You have six months to buy any additional Medicare coverage with no limitations to plan options. This is the best time to enroll since a carrier cannot deny you coverage due to any pre-existing health conditions.
Annons Find your best rate from over 4700 Medicare plans nationwide. Medicare is relied upon by millions of Americans including seniors 65 years of age or older and individuals under the age of 65 with certain disabilities. Dont Buy Meticore Unless Youve Seen This Massive Discount Exclusive Bonuses.