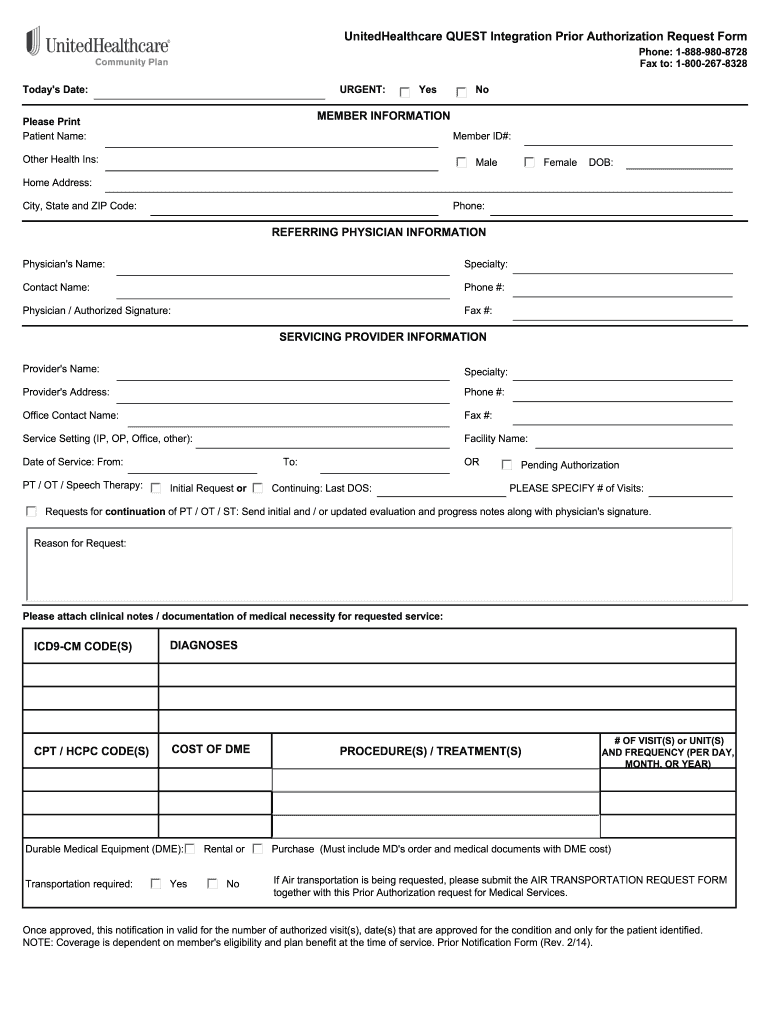
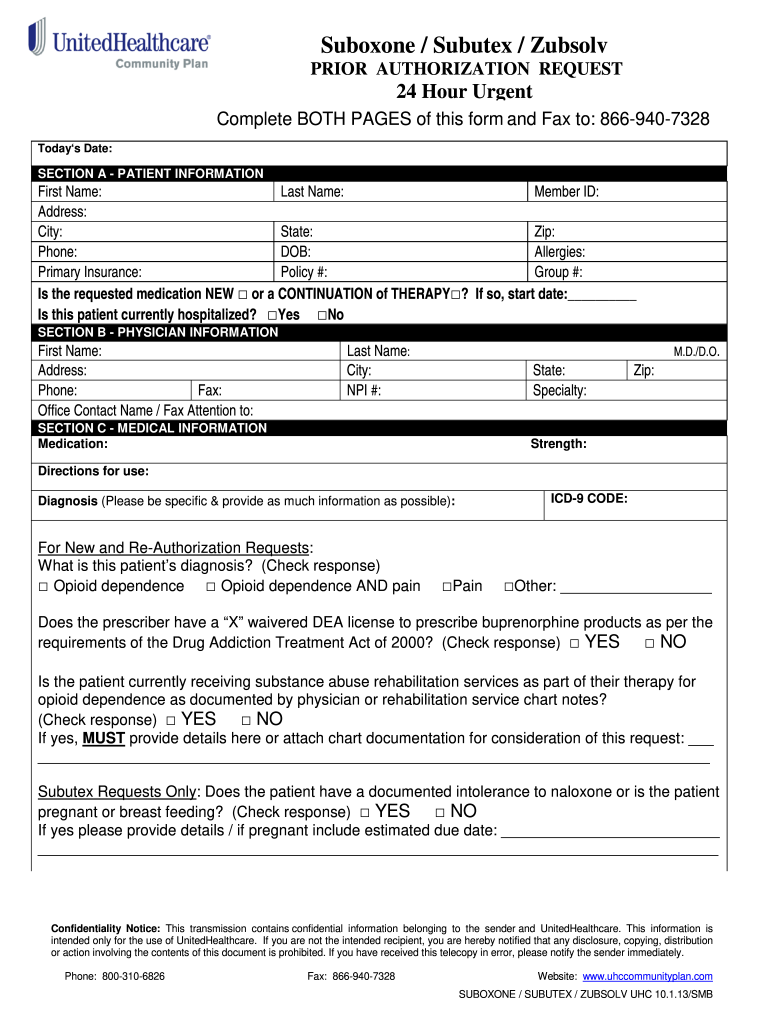
Prior authorization requests are defined as requests for pre-approval from an insurer for specified medications or quantities of medications before they are dispensed. How to Get Prior Authorization after the fact.
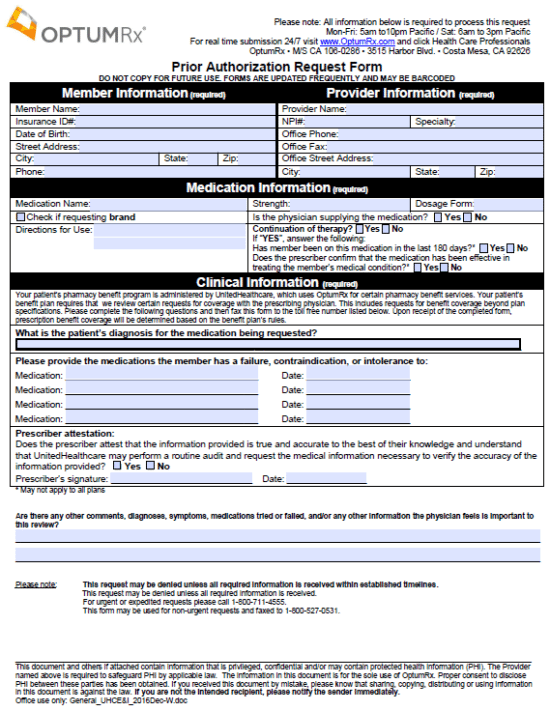 Optumrx Prior Prescription Rx Authorization Form Authorization Forms
Optumrx Prior Prescription Rx Authorization Form Authorization Forms
The process also allows your health insurance company to review your prescriptions looking for any potentially dangerous drug interactions that your doctor may have been unaware of when prescribing.
Prior authorization for prescription. Obtaining a prior authorization from the payer for the prescription FollowUpRequest originated from the pharmacy to. If you dont get prior authorization a medication. In addition to commercial issuers the following public issuers must accept the form.
Without this prior approval your health insurance provider may not pay for your medication or operation leaving you with the bill instead. Your insurance provider. Prior Authorization Request For Prescriptions Prescription requests may require prior authorization to be rendered.
Providence Prior Authorization Form Fax to. Labs must register their tests to participate as part of the Genetic and Molecular Lab Testing NotificationPrior Authorization process. In a document laying out suggested reforms AMA urged payers to ensure that prior authorization prescription programs are based on up-to.
The executive commissioner may require prior authorization for the reimbursement of a drug provided through any other state program administered by the commission or a state health and human services agency including a community mental health center and a state mental health hospital if the commission adopts preferred drug lists under Section 531072. Ordering care providers will complete the notificationprior authorization process online or over the phone. June 24 2019 - A new rule from CMS calls for electronic prior authorization ePA updates aiming to improve prescribers decision-making processes ease administrative burden and decrease the.
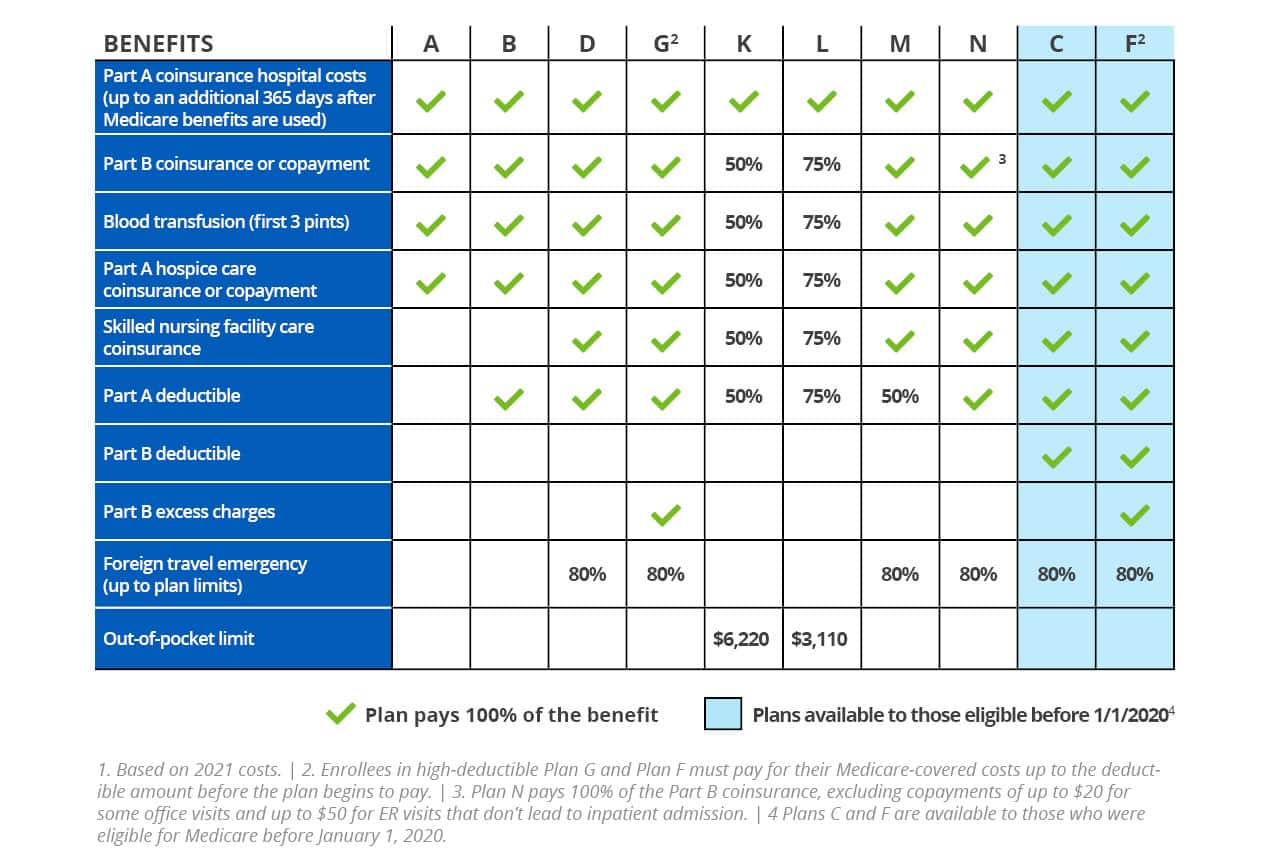
Prior authorization can help lower the cost of expensive prescriptions by first requiring you to try a lower cost alternative thats equally effective. Only be approved to treat specific conditions or cost more than other medications used to treat similar conditions. For Medicare Advantage Plan Members fax the completed form to 1-800-401-0915.
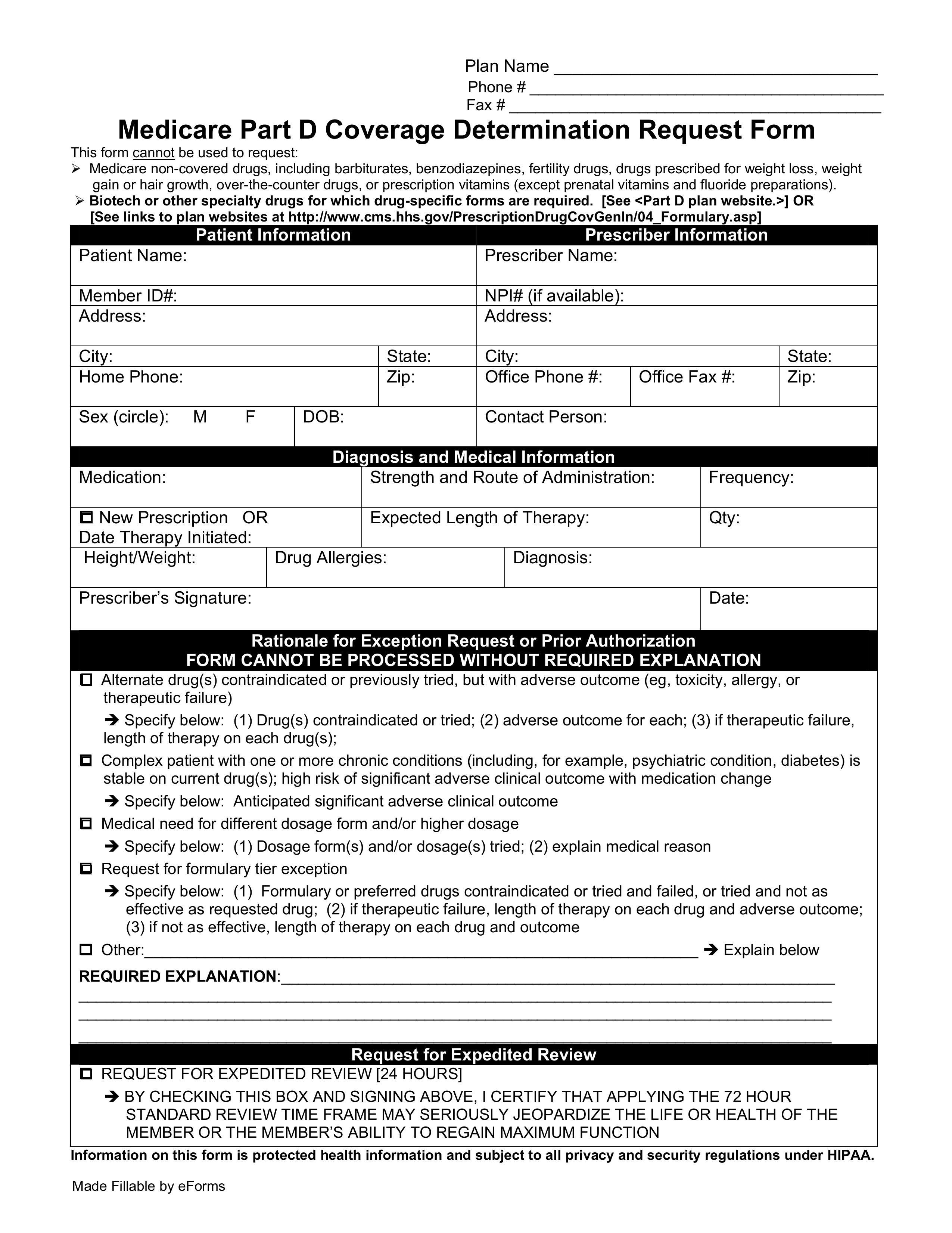
These factors can lead to customer service issues increased healthcare costsand even negative patient outcomes. Some medications must be reviewed because they may. The Medicare Prior Rx Authorization Form or Drug Determination Request Form is used in situations where a patients prescription is denied at the pharmacy.
Completed form to. We want to know if the medication is medically necessary and appropriate for your situation. The AMA believes that the overall volume of medical.
This means we need to review some medications before your plan will cover them. Prior authorization is a requirement that your physician obtains approval from your healthcare provider before prescribing a specific medication for you or to performing a particular operation. Your insurer will then decide whether or not to cover your medicine and you should hear back from your pharmacist about their decision within two days.
Remember if you are approved a prior. Learn more about the Genetic Molecular Lab Testing Notification Prior Authorization Process. Automate the prior authorization process.
Prior authorizationsometimes called precertification or prior approvalis a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage. Medicaid the Medicaid managed care program the Childrens Health Insurance Program CHIP and plans covering employees of the state of Texas most school districts and The University. All supporting medical documentation andor any additional pertinent information.
Prescription medications sometimes need prior authorization PA to determine if the HealthSelect SM Prescription Drug Program PDP administered by OptumRx can cover them. If you need to fill out a Providence prior authorization form for either medications or medical services you can download fillable PDF versions of these forms on this page and you will also find the fax numbers required for delivery purposes. What is prior authorization.
Prescriber means the term as defined in section 17708 of the Public Health Code 1978 PA 368 MCL. Once a patient or their physician receives a written denial coverage determination they should submit a coverage determination request form asking for the drug to be covered. Your pharmacy will contact if your doctor if he or she did not obtain prior authorization from the insurance.
The physician will contact the insurance company and submit a formal authorization request. Form for Prescription Drug Benefits if the plan requires prior authorization of a prescription drug or device. 1 503 574-8646 1 800 249-7714.
For all other Members fax the. Prescriptions that require prior authorization PA can delay treatment frustrate patients and increase pharmacy workload. Notify prescribers that this is a follow-up RxRenewalRequest or RxChangeRequest transaction when the prescriber has not responded to the first RxRenewalRequest or first RxChangeRequest transaction in a reasonable amount of time.
If your prescription requires a prior authorization the pharmacy will notify your healthcare provider who will provide the necessary information to your insurance company.