HUB OTP Buprenorphine Prior Authorization Form. Medically necessary To be medically necessary means it is appropriate reasonable and adequate for your condition.
 Free 8 Prior Authorization Form Samples In Pdf Ms Word
Free 8 Prior Authorization Form Samples In Pdf Ms Word
You may need prior authorization for your prescription if it.
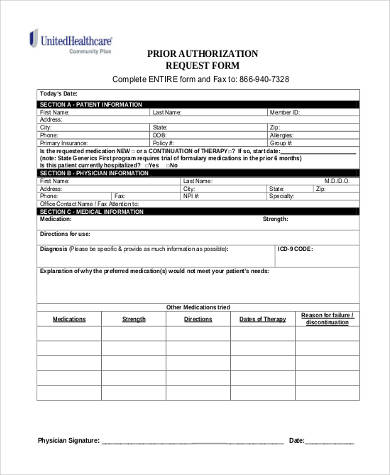
Prior authorization request form. General Prior Authorization Request Form. We use it to make sure your prescription drug is. When you do need to submit a request for a service that needs prior authorization please complete the form and submit all relevant clinical data such as progress notes treatment rendered tests lab results and radiology reports to support the request for services.
Certain requests for coverage require review with the prescriber. IHCP Prior Authorization Request Form Version 62 May 2021 Page 1 of 1 Indiana Health Coverage Programs Prior Authorization Request Form Fee-for-Service Gainwell Technologies P. There is no other equally effective.
Medical Necessity Supporting Documentation. Cimzia Prior Authorization Form. Use this form to request authorization by fax or mail when a n issuer requires prior authorization of a health care service.
The Medicaid prior authorization forms appeal to the specific State to see if a drug is approved under their coverage. Texas Standard Prior Authorization Request Form for Health Care Services Last Modified 08032018 Texas Specialty Programs Prior Authorizations. This form is made available for use by prescribers to initiate a prior authorization request with the health insurer.
The provider will have 60 days from the date of the claim denial to appeal and. To see which documentation is necessary for a prior authorization request. Some prior authorization requests require documentation in addition to the prior authorization form to support a determination of medical necessity.
Fax is not a secure method of transmission. Prior authorization requests are defined as requests for pre-approval from an insurer for specified. 800-687-0707 Fax back to.
Prior Authorization Forms and Policies. All other Medicaid requirements must be met in order for a. Allow at least 24 hours for review.
KanCare Medicaid Behavioral Health PRTF Prior Authorization Request Form. General Prior Authorization Forms. If you have questions please call 800-310-6826.
Before completing this form please confirm the patients benefits and eligibility. Please submit your request to the fax number listed on the request form with the fax coversheet. Information contained in this form is Protected Health Information under HIPAA.
844-370-6203 MaxorPlus manages the pharmacy drug benefit for your patient. Prior authorization does not guarantee reimbursement. HOW LONG IS THIS PROBLEM EXPECTED TO LAST.
This form may contain multiple pages. I certify that the information given in this form is a true and accurate medical indication for the procedures required. Provider to receive reimbursement.
Is specified by the DoD Pharmacy. Benefits for services received are subject to eligibility and plan terms and conditions that are in place at the time services are provided. Please complete all pages to avoid a delay in our decision.
Policies may vary between each states department of health but the process more. Prior Authorization Request Form Medica requires that providers obtain prior authorization before rendering services. _____ Type of PA.
Prior Authorization Request Form Please complete this entire form and fax it to. Authorization and Notification Resources Prior Authorization Paper Fax Forms. Buprenorphine Spoke OBOT Prior Authorization.
Please answer the following questions and fax this form to the number listed above. Opens a new window or tab. This pre-authorization request form should be filled out by the provider.
Problem resulting from the diagnosis which relates to this prior authorization request. Use the Online Prior Authorization and Notification tool KanCare Medicaid Behavioral Health Inpatient Prior Authorization Request Form. Indiana Standard Prior Authorization Request Form for Health Care Services Please note.
Antipsychotic Medications Pediatric Age Prior Authorization Form. This form is to be completed by the patients medical office to see if he or she qualifies under their specific diagnosis and why the drug should be used over another type of medication. If any items on the Medica Prior Authorization list are submitted for payment without obtaining a prior authorization the related claim or claims will be denied as provider liability.
Pre-authorization fax numbers are specific to the type of authorization request. 1-800-457-4584 option 7 F. Prior Authorization Prior authorization is a routine process.
Botulinum toxin injection. An Issuer may also provide an electronic version of this form on its website that you can complete and submit electronically through the issuers portal to request prior authorization of a health care service. Pharmacy Prior Authorization Request Forms and Order Forms.
_____ MONTHS INDEFINITELY PERMANENTLY. Member Information Prescriber Information Member Name. This will help us process your request.
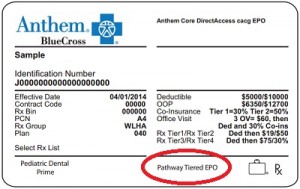
Instructions Complete this form fully and legibly. 1-800-689-2759 Hoosier Healthwiseauthorize the Anthem Hoosier Healthwise P. PRIOR AUTHORIZATION REQUEST FORM EOC ID.
Prior Authorization PA Request Form Submit the prior authorization request form along with supporting documentation to WPS Government Health Administrators GHA Date of Submission.