Medicare and Medicaid in some states cover proton therapy and Blue Cross Blue Shield of Mississippi has at times approved the treatment. Blue Shield of California has notified 300 radiation oncology and urology practices in the state that as of the end of October it will no longer cover proton-beam therapy for prostate cancer.
 University Hospitals Is Hitting Mark With Proton Therapy
University Hospitals Is Hitting Mark With Proton Therapy
BCBSTX covers all medically necessary care that Medicaid covers.

Does blue cross blue shield cover proton therapy. Visits to PCPs specialists with an OK ahead of time for out-of-network providers or other providers. Some studies using proton beam therapy in pediatric central. Some proton therapy centers such as the University of Pennsylvania Mayo Clinic and University of Maryland have sometimes set the price of proton therapy equal to intensity-modulated radiation therapy while evidence is being developed.
CIGNA Proton Beam Therapy for Ocular Melanoma Ocular Hemangiomas. Physical speech and occupational therapy. This policy will be applied as a part of AIM Clinical Guidelines beginning November 1 2018.
Evidence is lacking on the definition of age parameters for the use of proton beam therapy in pediatric patients. You wont pay a copay or coinsurance for these services and you dont need to meet your deductible before you use these services. In Texas a new pilot program between The University of Texas Systems employee benefit program Blue Cross Blue Shield of Texas and The University of Texas MD.
Supply is medically necessary does not constitute a representation or warranty that the Blue Cross and Blue Shield Service Benefit Plan covers or pays for this service or supply for a particular member. The law does not explicitly require insurers to cover proton beam radiation therapy but it bars them from holding the cancer treatment to a higher standard than they would any other type of. Adult physicals and blood pressure and cholesterol screenings.
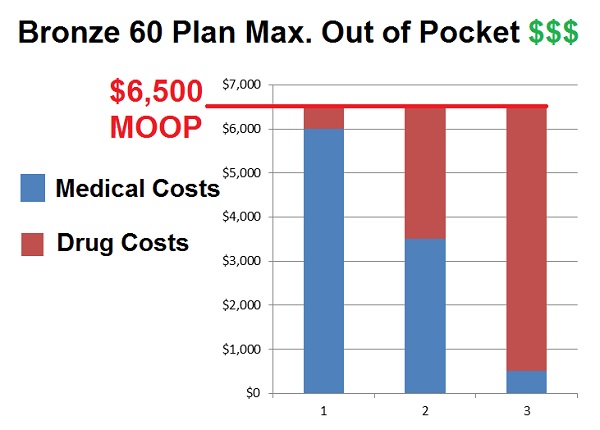
This chart is a. Some insurers including Cigna Independence Blue Cross and Blue Cross Blue Shield of Florida cover proton therapy for selected cancers being studied sometimes with study participation. Submit to your Local Plan Complete the Clinical Exception and Notification Form for BCBSMA Medical Policy 437 Charged-Particle Proton or Helium Ion Radiation Therapy.
CIGNA Proton Beam Therapy for Intracranial and Skull Base Tumors Unknown CIGNA HealthCare covers proton beam therapy as medically necessary for the treatment of intracranial and skull base tumors when radiation therapy is indicated and recommended by the treating physician. All plans also offer preventive services at no charge. Yearly adult well exams.
Physicians not insurance companies should. Anthems coverage guideline THER-RAD000002 Proton Beam Radiation Therapy will be archived effective November 1 2018. But these payment policies are.
Online access is available 247 to process orders in real-time and is the fastest. This program will not apply to members who are -insured administrative covered through self services only ASO plans nor will it apply to any members of other Blue Cross andor Blue Shield Plans that may access the above networks through the BlueCard program. Which radiation oncology services require a prior authorization.
But Hierlmeier was denied three times. Blue Cross Blue Shield covered proton therapy for prostate cancer until April of last year and now inexplicably it will not Yonemoto said. Clarified proton beam therapy appropriate for all pediatric tumors requiring radiation therapy.
Deputy Commissioner Rhoads says hes heard the complaint that private insurers in Oklahoma - Blue Cross-Blue Shield primarily are indiscriminately denying coverage of proton therapy and says the. Plus Regence Blue Cross Blue Shield Highmark and Blue Cross Blue Shield of Kansas City all have already stopped covering the treatment the WSJ noted. Routine physicals for children from birth through 20 years of age.
August 2018 Anthem Provider Newsletter --. All services must be medically necessary. Blue Cross Blue Shield of Massachusetts PO Box 986065 Boston MA 02298 Services rendered outside of Massachusetts.
As a reminder ordering and servicing providers may submit prior authorization requests to AIM in one of several ways. In addition the chart below tells you about the benefits covered by this plan. He said the new state law specifically says it cannot be read as requiring insurers to cover proton therapy but that the companies should use the same clinical standards to.