To Whom It May Concern. The basics of obtaining an authorization for assessment are usually simple.
 How To Obtain Prior Authorizations Jdrf
How To Obtain Prior Authorizations Jdrf
If the procedure is done or the drug prescribed before the insurance plan approves it.

How to get pre authorization from insurance company. Pre-approval rules vary from one health insurer to another but in general the more expensive the service the more likely it is that the insurer will require pre-approval. Your health insurance company will review your doctors recommendation and then either approve or deny the authorization request. A pre-authorization or pre-approval is a prior approval given by insurance companies to the Network Hospital or clinic Providers before certain health services can be availed by the member.
This means that you or your doctor must contact your insurer to obtain their approval prior to receiving care. The physician will contact the insurance company and submit a formal authorization request. Once the patient is scheduled for a procedure or a healthcare service you should initiate the verification process and enquire with the insurance company whether this particular procedure or service requires pre-authorization or not.
Service is evidence-based and is medically necessary in order to ensure that Beneficiary can communicate effectively. Health insurance companies use the prior authorization or pre-approval process to verify that a certain drug procedure or service is medically necessary BEFORE it is done or the prescription is filled. And 3 submitting a request for those services to the insurance company and waiting for the request.
I am writing to request pre-approval for service by name of provider. In some cases your insurance company will ask for more information from your doctor in order. There are three basic steps in the initial authorization process which can vary from plan to plan.
1 verifying the patients personal information including who their insurer is and what benefits they are entitled to receive. As mentioned in the How does prior authorization work section above this will then often prompt a time-consuming back and forth between the provider and payer. Usually they will communicate with your health insurance company.
Your insurer will then decide whether or not to cover your medicine and you should hear back from your pharmacist about their decision within two days. At 7 business days after the request has been first sent another phone call will be made to the insurance company to request status and at that time a phone call will be made to the patient to inform them of potential disruption in services if the insurance doesnt approve the requested visits within 3 days and encourage the patient to contact the insurance company. How do I get a prior authorization.
This is extremely important to know especially for people being treated for cancer. So things like surgery or hospital visits are more likely to need. 2 determining the patients home care needs.
Remember if you are approved a prior. If the company says it is required initiate the pre-authorization. How to Get Prior Authorization after the fact.
Your pharmacy will contact if your doctor if he or she did not obtain prior authorization from the insurance. The procedure of obtaining pre-authorization for an eligibility verification company or doctors office starts with the insurance verification process. Insurance companies will sometimes authorize a short-term supply eg three days to a week of a prescription while a PA is in process.
The representative may ask for notes from the chart Generally the insurance company will give you the authorization while on the phone or it may be obtained on-line. The healthcare provider is usually responsible for initiating prior authorization by submitting a request form to a patients insurance provider. You may need to call into an authorization department or send information via fax yesfax.
To get prior authorization. However it is your responsibility to make sure that you have prior authorization before. If the company says yes prior authorization is require ask them to get one started.
If your prescription requires a prior authorization the pharmacy will notify your healthcare provider who will provide the necessary information to your insurance company. Health care providers usually initiate the prior authorization request from your insurance company for you. Consult your plan documents or talk to a member services representative or your doctors office staff to find out what is needed to obtain an expedited approval.
I have reviewed my policy and believe that name of health care plan is required to cover this service. Have your office Tax ID number NPI number and the patients chart available. Some insurance companies will have a form you need to fill out and you will often need to submit the childs diagnostic report.
Your insurance provider. Review your Summary of Benefits and Coverage Document for more information about which services or supplies require prior authorization. Your doctor will start the prior authorization process.
 What Is Prior Authorization Why Do Insurance Companies Require It Academic Healthplans
What Is Prior Authorization Why Do Insurance Companies Require It Academic Healthplans
 How To Get Medical Pre Approval Or Prior Authorization Effectively
How To Get Medical Pre Approval Or Prior Authorization Effectively
 How To Get Pre Authorization From Insurance Company Motivasi My Id
How To Get Pre Authorization From Insurance Company Motivasi My Id
How To Obtain Health Insurance Prior Authorization In 3 Minutes Or Less
 How To Get Medical Pre Approval Or Prior Authorization Effectively
How To Get Medical Pre Approval Or Prior Authorization Effectively
 Importance Of Preauthorization In Revenue Cycle Management Rcm
Importance Of Preauthorization In Revenue Cycle Management Rcm
 The Ultimate Guide To Prior Authorization Myndshft
The Ultimate Guide To Prior Authorization Myndshft
 The Ultimate Guide To Prior Authorization Myndshft
The Ultimate Guide To Prior Authorization Myndshft
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
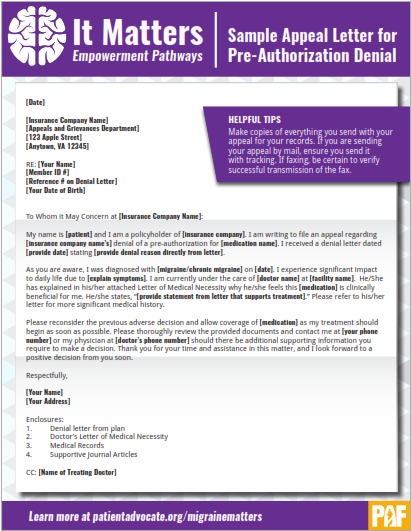 Sample Appeal Letter For Pre Authorization Denial Patient Advocate Foundation
Sample Appeal Letter For Pre Authorization Denial Patient Advocate Foundation
 How To Get Medical Pre Approval Or Prior Authorization Effectively
How To Get Medical Pre Approval Or Prior Authorization Effectively
 How To Get Preauthorization From Insurance Companies
How To Get Preauthorization From Insurance Companies
 Prior Authorization How Do You Get Insurance Companies To Approve Medications Youtube
Prior Authorization How Do You Get Insurance Companies To Approve Medications Youtube
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.