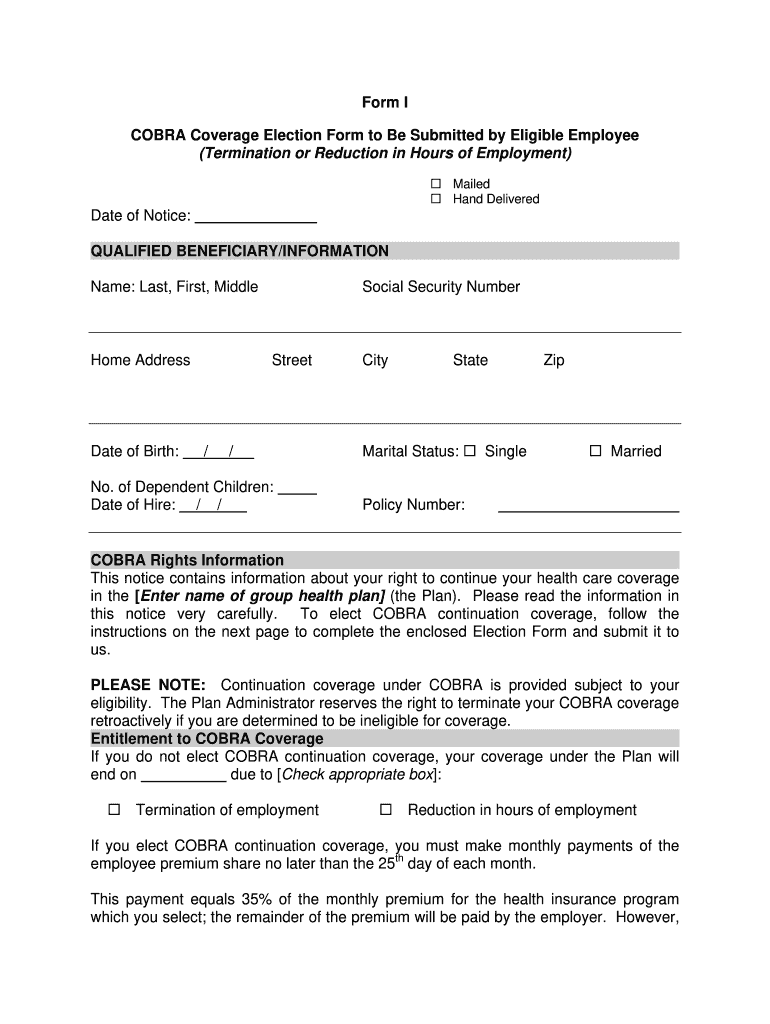
See Instructions - if completing by hand use. I understand that if I elect continuation coverage and I fail to pay any premium payment on time this coverage will terminate.
 Cobra Letter To Employee 2020 Template Fill Online Printable Fillable Blank Pdffiller
Cobra Letter To Employee 2020 Template Fill Online Printable Fillable Blank Pdffiller
I also agree to notify the Plan Administrator.
Cobra election form. Your Kaiser Permanente Representative can assist you in arranging continuation coverage for your COBRA-eligible employees. This notice must be provided within 14 days after the plan receives notice of the qualifying event. When the plan receives a notice of a qualifying event it must give the qualified beneficiaries an election notice which describes their rights to continuation coverage and how to make an election.
If you dont submit a completed Election Form by the due date shown above you may lose your right to elect COBRA continuation coverage. If you have not yet elected COBRA continuation coverage you may send this form along with your Election Form. Under the American Rescue Plan Act you have sixty 60 days after the date of this notice to decide whether you want to elect continuation coverage.
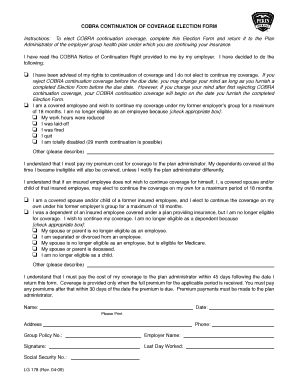
Social Security number or. COBRA CONTINUATION COVERAGE ELECTION FORM PLEASE PRINT Name COBRA Applicant SSN COBRA Applicant Mailing Address Street City State ZIP Code Date of Birth Marital Status Phone Gender Male Female Coverage elections please check the box next to the coverages you would like to continue. If mailed it must be post-marked no later than enter date.
Section 1 NOTIFICATION To be completed by the EmployerPlan Administrator 1. To elect continuation coverage complete this online Election Form. If you are already enrolled in COBRA you may send this form in separately.
Please retain a copy of the completed Election Form for. FAQs About COBRA Continuation Health Coverage. If you reject COBRA continuation coverage before the due date you may change your mind as long as you submit a completed Election Form.
The election form makes a subtle reference to the outbreak period relief by suggesting some qualified beneficiaries may have additional time to elect due to a national emergency. HDS COBRA ELECTION FORM 04_21. Final regulations on the COBRA notice provisions of Part 6 of Title I of ERISA.
If you dont submit a completed Election Form by the due date shown above you may lose your right to elect COBRA continuation coverage. Tips on how to fill out the Cobra election form 2013-2019 on the web. This period is measured from the later of the date of the qualifying event or the date the COBRA election notice is provided.
I have read this form and the notice of my election rights. However if qualified beneficiaries want to receive the COBRA subsidy they must elect. For faster service you may fax the completed form to 515-376-9043.
If you reject COBRA continuation coverage before the due date you may. Form within 31 days of enrolling in health coverage and whenever the status of tobacco use changes for you or a dependent covered under your health insurance. COBRA Administrator Station 3W395 PO Box 9232 Des Moines IA 50306-9232 If you are submitting a premium payment at this time please attach to the Election Form.
You dont have to. This Election Form must be completed and returned by mail or describe other means of submission and due date. If mailed it must be post-marked no later than enter date.
COBRA NOTICE OF ELECTION NOE SOUTH CAROLINA PUBLIC EMPLOYEE BENEFIT AUTHORITY. The sample election form on the front may be photocopied for use if your company has not developed one. Model election notice En Español.
How long do I have to elect COBRA coverage. Employee Name If different. HDS Dental Termination Date.
An Employees Guide to Health Benefits Under COBRA. Qualified beneficiaries must be given an election period of at least 60 days during which each qualified beneficiary may choose whether to elect COBRA coverage. ACA Implementation FAQs Part 32.
COBRA Coverage Election Agreement. The advanced tools of the editor will lead you through the editable PDF. Mail your completed Election Form to.
If you dont submit a completed Election Form by the due date shown above youll lose your right to elect COBRA continuation coverage. The Department considers appropriate use of the model election notice to be good faith compliance with the election notice content requirements of COBRA and the American Rescue Plan Act of 2021 ARP. If you do not complete this form and return it within 60 days of receipt you may be unable to receive the premium assistance.
To use this model election notice properly the Plan Administrator must fill in the blanks with the appropriate plan information. The election form included with the model notice informs qualified beneficiaries that they have 60 days from the date of the notice to elect COBRA coverage. This Election Form must be completed and returned by mail.
I understand my rights to elect continuation coverage and would like to take the action indicated below. If you do not submit a completed Election Form by the June 30 2021 you will lose your right to elect continuation coverage. This Election Form must be completed and returned by mail or describe other means of submission and due date.
COBRA PREMIUM ASSISTANCE SPECIAL ENROLLMENT ELECTION FORM INSTRUCTIONS. Questions regarding further details of the law should be addressed by your legal counsel or benefits. If you reject COBRA continuation coverage before the due date you may change your mind as long as you submit a completed Election Form.
Under the American Rescue Plan Act of 2021 you are only entitled to elect COBRA Coverage at this time if you lost group health plan coverage due to an involuntary termination of employment or reduction of hours during the period that begins with April. To start the document utilize the Fill Sign Online button or tick the preview image of the document. COBRA coverage is retroactive if elected and paid for by the qualified beneficiary.
It must be post-marked no later than enter date.




/domestic-partner-insurance-101-2645680_final-aa4fc77cbbca4103a52bbbad3c906435.png)