Virtual visits are covered and standard office visit copays may apply based on your plan benefits. An Independent Licensee of the Blue Cross and Blue Shield Association.
Http Pages Natera Com Hubfs Panorama Cta Content Panorama Insurance Coverage 16 10 10 Pdf
Enrollment in Blue Cross Blue Shield of Massachusetts depends on contract renewal.
Does blue cross blue shield cover panorama test. Waiving cost-sharing for COVID-19 testing and treatment. A bone density test is used mainly to diagnose osteopenia and osteoporosis. How much did your NIPT cost specifically Panorama.
Its also used to determine your future fracture risk. Benefits Application This medical policy relates only to the services or supplies described herein. Exact Sciences Laboratories LLC is independent from and not affiliated with Horizon Blue Cross.
File is in portable document format PDF. Yes CareFirst Blue Cross Blue Shield requires documentation to cover CPAP therapy supplies. Contact your primary healthcare provider to find out if they have virtual visits available.
Also depending on your health plan and provider you may be able to. They review your situation and determine coverage on a case by case basis so you could end up paying 700 or you could end up paying 99. BCBSNC will provide coverage for Testosterone Testing when it is determined to be medically necessary because the medical criteria and guidelines shown below are met.
Next generation sequencing NGS panel testing of either Ashkenazi Jewish related disorders panel or panethnic carriers screening panel of 15 tests as long as a single appropriate AMA genetic sequencing procedure test code is submitted 4. Carrier screening See Note 1 below of the biological father may be covered. Please refer to the Members Benefit Booklet for availability of benefits.
One option is Adobe. They do self pay prices which are 250-300 out of pocket if youre interested. Unfortunately it is one of those things where you dont know until after you get the test.
Tests for DMHC-defined essential workers without symptoms or known or suspected exposure will also be covered if you are enrolled in a DMHC individual family or group plan. Exact Sciences Laboratories LLC is an independent company that supports Horizon Blue Cross Blue Shield of New Jersey in administration of Cologuard testing for covered members. With no cost to the member Blue Cross will pay for the appropriate medically necessary testing and in-network care including hospitalization for fully insured 1 employer individual and Medicare members.
What virtual care options does my plan cover. Waiving all prior authorization requirements for COVID-19 testing and related covered services. As part of our mission to improve and protect the healthcare system particularly under the threat of the CoronavirusCOVID-19 the Blue Cross Blue Shield Association is focused on protecting members from fraudsters who seek to take advantage of the fear and confusion many feel surrounding the coronavirusCOVID-19 during these uncertain times.
Cologuard is a registered trademark of Exact Sciences Laboratories LLC. Drug testing coverage is limited to 20 tests per the calendar year unless the insured seeks special approval. But it is not as precise as the nonportable methods because only 1 bone.
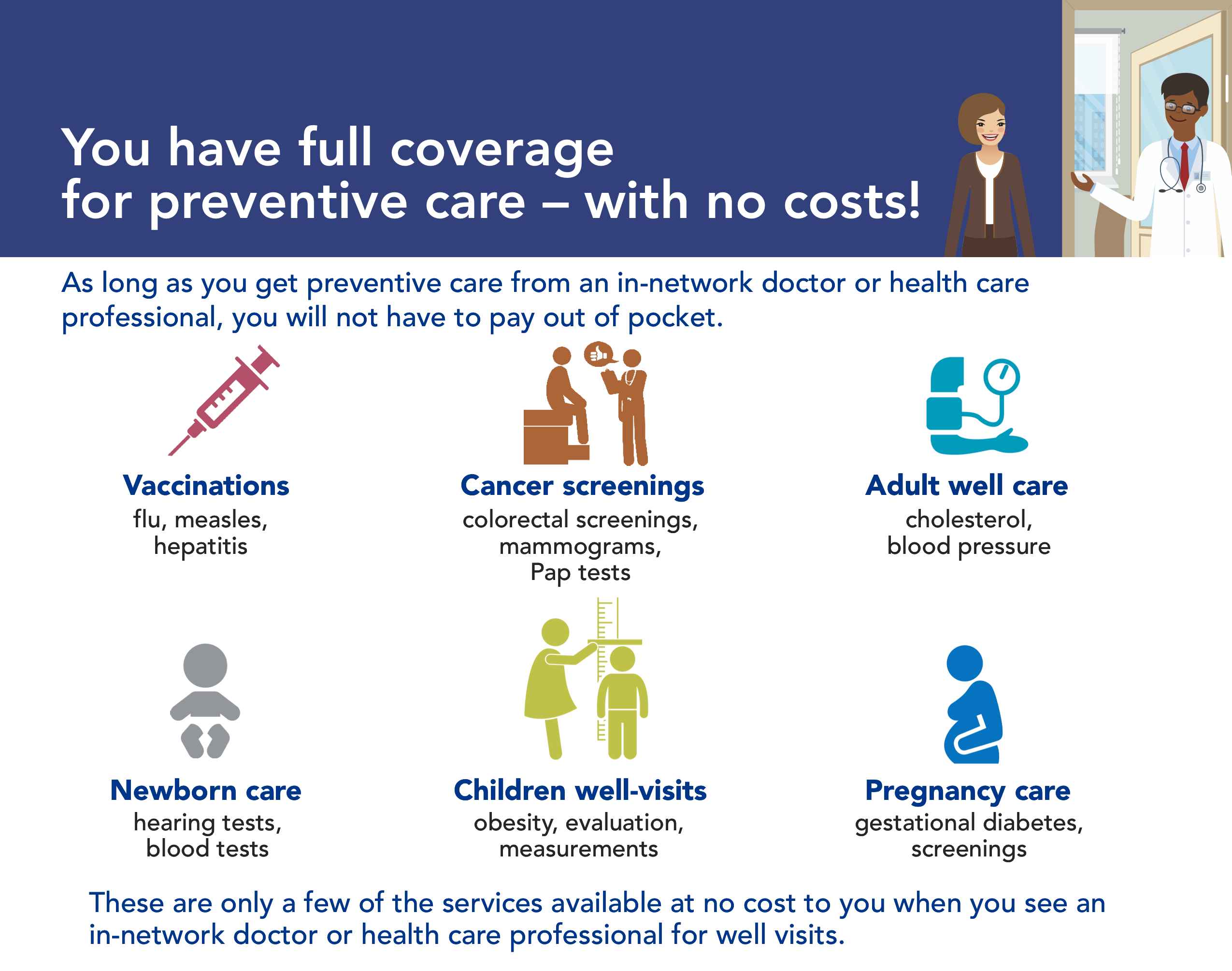
Apparently only if youre over 35 though. Most PDF readers are a free download. Your BCBSTX health plan may cover preventive services like your annual exam when you see an in-network doctor.
My doctor warned me that this test could cost several thousands out of pocket. Blue Cross Blue Shield insurance does cover testing. Blue Cross Blue Shield Federal Blue Cross Blue Shield Illinois Blue Cross Blue Shield Kansas City Blue Cross Blue Shield Massachusetts Blue Cross Blue Shield Michigan Blue Cross Blue Shield Minnesota Blue Cross Blue Shield Nebraska Blue Cross Blue Shield North Carolina Blue Cross Blue Shield North Dakota Blue Cross Blue Shield Rhode Island Blue Cross Blue Shield South Carolina Blue Cross Blue Shield Texas Blue Cross Blue Shield.
This documentation includes relevant doctors notes sleep test results a prescription among other items. One said specifically they accept my insurance. Blue Cross will cover the full cost of testing in-network care and vaccine administration related to COVID-19.
They could cover it they could not. My insurance wont cover it. Items that are covered include the following.
Members benefits may vary according to benefit. Panorama has said they offer a cash price of 249-349. Some plans may also have access to Teladoc Heal or NurseHelp 247 as alternative options for virtual care.
These services can help you see if your symptoms may be. To view this file you may need to install a PDF reader program. Portable testing may use the radius 1 of the 2 bones of the lower arm wrist fingers or heel for testing.
Only tests ordered by a healthcare provider licensed to order COVID-19 tests will be covered by Blue Shield and Blue Shield Promise at no out-of-pocket cost to you. Blue Cross Blue Shield of Massachusetts is an HMO and PPO Plan with a Medicare contract. I dont have blue cross blue shield but I got pamphlets for 3 different NIPT tests which are the major ones they offer.
These members will not have any copay coinsurance or deductible costs for COVID-19 testing. That means members will pay nothing out-of-pocket to take care of their COVID-19-related health needs. The Blue Cross Blue Shield companies partner.
Prenatal Screening AHS G2035. An annual exam is a yearly preventive visit with your doctor to check your physical and mental health. The test typically measures the bone density of the bones of the spine lower arm and hip.
Anthem Insurance Companies Inc Blue Cross and Blue Shield of Massachusetts Inc Blue Cross Blue Shield of Rhode Island and Blue Cross and Blue Shield of Vermont are the legal entities that have. Telligent is an operating division of Verint Americas Inc an independent company that provides and hosts an online community platform for blogging and access to social media for Blue Cross and Blue Shield of Texas.