Requirements for Pre-Approval of Weight Loss Surgery with Blue Cross Your Anthem Blue Cross insurance policy covers weight loss surgery unless it states specifically that it excludes it. You need must be between the ages of 18 and 60 years old.
Http Mcgs Bcbsfl Com Mcg Mcgid 02 40000 10 Pv False
The policies contained in the FEP Medical Policy Manual are developed to assist in administering contractual benefits and do not constitute medical advice.
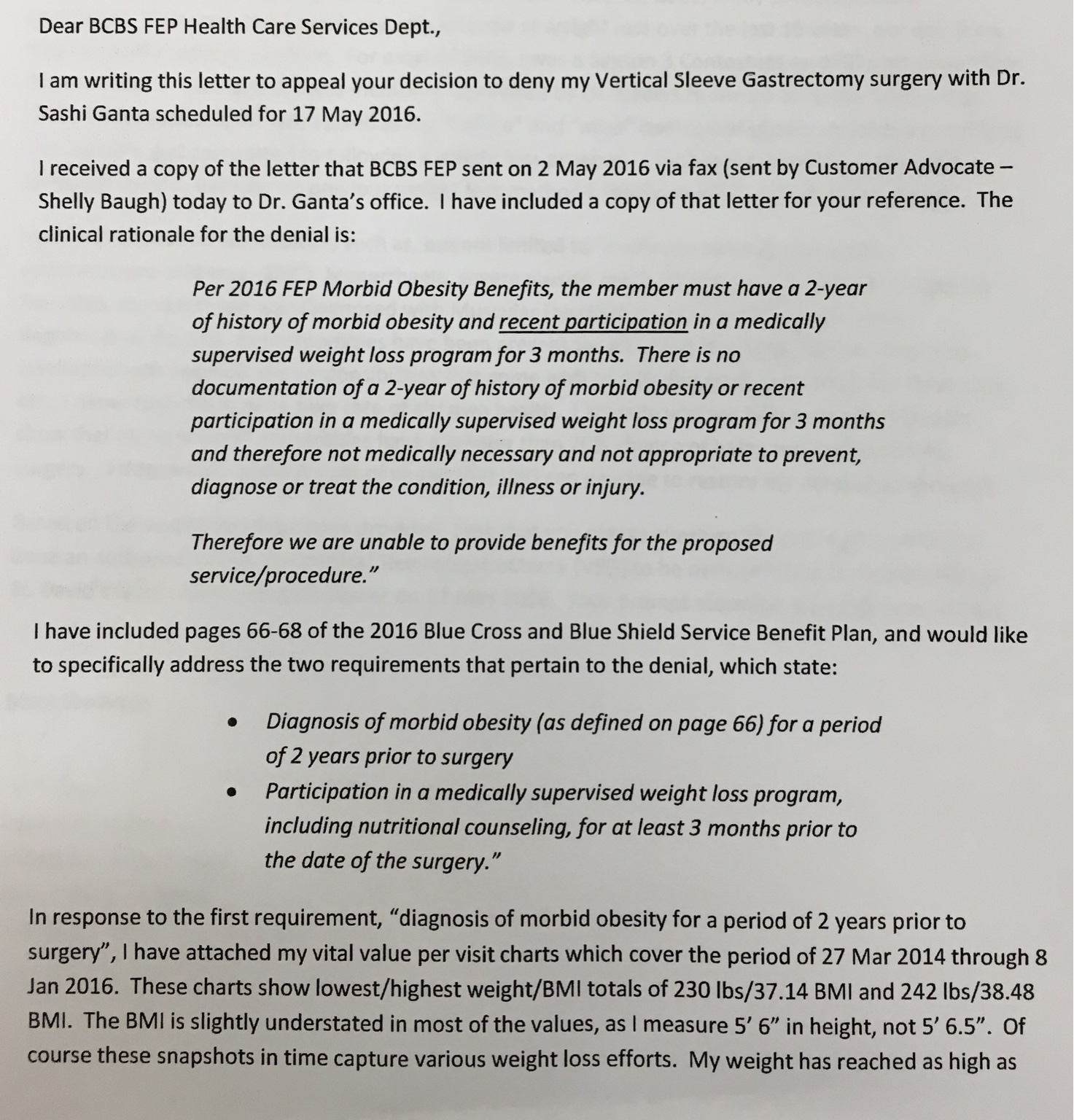
Bcbs fep bariatric surgery requirements 2019. Some bariatric procedures may include both a restrictive and a malabsorptive component. Up to 875 per admission Outpatient. The 2019 Clinical practice guideline developed by the AACEACE The Obesity Society American Society for Metabolic Bariatric Surgery ASMBS Obesity Medicine Association and American Society of Anesthesiologists addresses the nonsurgical support of those who will be undergoing bariatric procedures Mechanick 2019.
Just wondering if anyone had any experience with getting an approval through FEP Blue. Physiciansurgeon fees 30 coinsurance Not covered certain surgical services. I have finished all of the requirements and my surgeons office is going to submit the request and curious as to what the turn around time is for the approval.
Stay Prior approval is required for Facility fee eg hospital room 30 coinsurance Not covered Precertification is required. Bariatric procedures remain a safe and effective intervention for higher-risk pa-tients with obesity. It is a choice for some people who are obese and have not been able to lose weight with other methods.
Blue Cross Blue Shield Global Core. Bariatric surgery is a type of surgery to help you lose weight. 1 gastric -restrictive procedures that create a small malabsorptive procedures which produce weight loss due to malabsorption by altering the normal transit of ingested food through the intestinal tract.
Bariatric weight loss surgery is considered not medically necessary for patients with a BMI less than 35 kgm. Body Mass Index of 40 or greater OR BMI 35 or more with comorbidities. Performing surgeon for surgical procedures performed in an office setting.
Your provider will document the place of service when filing your claim for the. 200 copayment per performing surgeon for surgical procedures performed in all other settings. 5 feet 5 inches.
Documentation of failed diets by conservative treatment. More than one-third of Americans are obese and while more than 250000 bariatric surgeries are performed annually in the United States experts say surgery. Evaluation from a professional counselor psychologist or psychiatrist within 12 months prior to surgery.
ER accidental injury 175 per day per facility ER medical emergency. A body mass index BMI of 40 or more OR a BMI between 30 and 399 with a serious obesity-related health problem like diabetes high blood pressure sleep apnea high cholesterol joint problems or others OR a BMI of 30 to 40 with or without health issues for the gastric balloon procedure. In order to be pre-approved for the procedure you must meet the following requirements.
100 per day per facility 1. And have been previously unsuccessful with medical treatment for obesity Commercial Products. Federal Employee Program FEP.
Inpatient Precertification is required. Posted June 20 2013. They are not intended to replace or substitute for the independent medical judgment of a practitioner or other health care professional in the treatment of an individual member.
You are at least 18 years of age and fully grown. Quality Selection Criteria for Ambulatory Surgery Centers Bariatric Surgery Program Accreditation by the Metabolic and Bariatric Surgery Accreditation. The minimum bariatric surgery qualifications include.
For a current list of Blue Distinction Centers for bariatric surgery use the BCBS Blue Distinction Facility Search tool. The site of service for bariatric surgery must be a Blue Distinction Center for Specialty Care BDSC. Posted July 18 2019.
Documentation attesting that you understand the post-operative regimen. Introduction This 2019 clinical practice guideline CPG update pro-vides revised clinical management recommendations that. Enhanced recovery after bariatric surgery procedures are discussed in detail.
BCBS Federal Employees Program Pre-Approval Requirements The items below are the minimum necessary for approval of your weight loss surgery. Ive been doing lots of research on the VSG and I feel it is my best long-term weight loss option. 200 in a non-office setting 1.
Bariatric type surgery to treat conditions other than morbid obesity Adjustable gastric banding gastric bypass using a Roux-en-Y anastomosis or sleeve gastrectomy is considered. We will reduce benefits for the inpatient hospital stay by 500 if no one contacts us for precertification. Bariatric surgery for HMO members only.
Im new to this entire process. A bodymass index 35 or Have at least one co-morbidity related to obesity. Bariatric surgery falls into two general categories.
Bariatric surgery for a BMI less than 35 kgm. Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies. Comply with applicable federal civil rights laws and do not exclude people or treat them differently on.
Documentation from the requesting surgeon that. MEDICAL CRITERIA BlueCHiP for Medicare Bariatric surgery is covered when the following criteria are met. Surgery 150 in an office setting 1.
There is a 100 penalty if prior. For benefits and limits call 602 -864 4320 1. Blue Distinction Centers for Bariatric Surgery Program Selection Criteria Table 3.