25 Generic 75 Preferred Brand 100 NonPreferred Brand. CVSCaremark is here to help you understand your prescription benefit plan so you can save time and money.
 Afspa Foreign Service Benefit Plan Prescription
Afspa Foreign Service Benefit Plan Prescription
Just like your medical plan covers visits to your doctor your Express Scripts prescription plan covers the medication your doctor prescribes.

Prescription benefit plan. Many translated example sentences containing prescription benefit plan French-English dictionary and search engine for French translations. Were the largest independent pharmacy benefit manager PBM and one of the biggest pharmacies in the US. At FBG Rx our mission is to offer superior prescription benefit services that balance the needs of our clients.
Prescription Benefits Prescription Drug Coverage. Whatever level of coverage you elect under your medical plan will apply to the Prescription Benefit Plan as well. Pharmacy benefits and services from Aetna can help individuals and families make the best choices for their health and budget.
You and inVentiv Health share in the cost of your coverage. A Nationwide Pharmacy Network. Your portion of the cost is.
You sign up and go to the pharmacy pay a small co-pay and go home. A 200person retail-only calendar year prescription drug deductible. Members who use the PBMs pharmacy network to obtain their medication will be charged the applicable prescription copayment after the prescription deductible has been met.
People who have this coverage will need to pay an annual deductible and monthly premium in order to take advantage of the benefits and people will need to pay a co-pay for any individual prescription. Or check with your employer. Unfortunately for seniors the donut hole still exi.
Plan Benefit Option Learn about your prescription plan drug coverage and all your savings options. Paying for Prescription Benefit Coverage The cost of the Prescription Benefit Plan is included in the cost of the inVentiv m edical plan you choose. Check availability and costs Price a drug and see a list of your Plans preferred list to save money.
We serve more than 85 million people. These are medications you take for chronic conditions such as high blood pressure asthma diabetes and high cholesterol. Please contact your Employer or refer to your ID Card to see which Rx Option you are enrolled in.
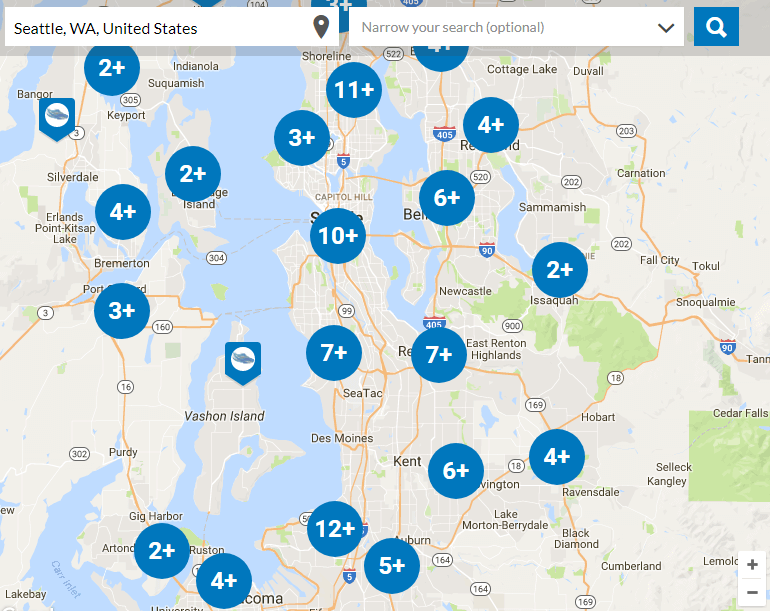
Prescription Benefit Plan Summary Members Health Plan NJ Offers Its Members Comprehensive Pharmacy Coverage Through Aetna The following Prescription Drug Benefit Section applies for all Plans that have elected Prescription Coverage. Specialty 90 day max supply. You can search for a local pharmacy here.
When getting medication from your neighborhood participating pharmacy you can. Prescription Benefit Plans seem easy. The most effective way of using your Prescription Drug benefit for short-term medication is with the prescription drug card issued by the Plan.
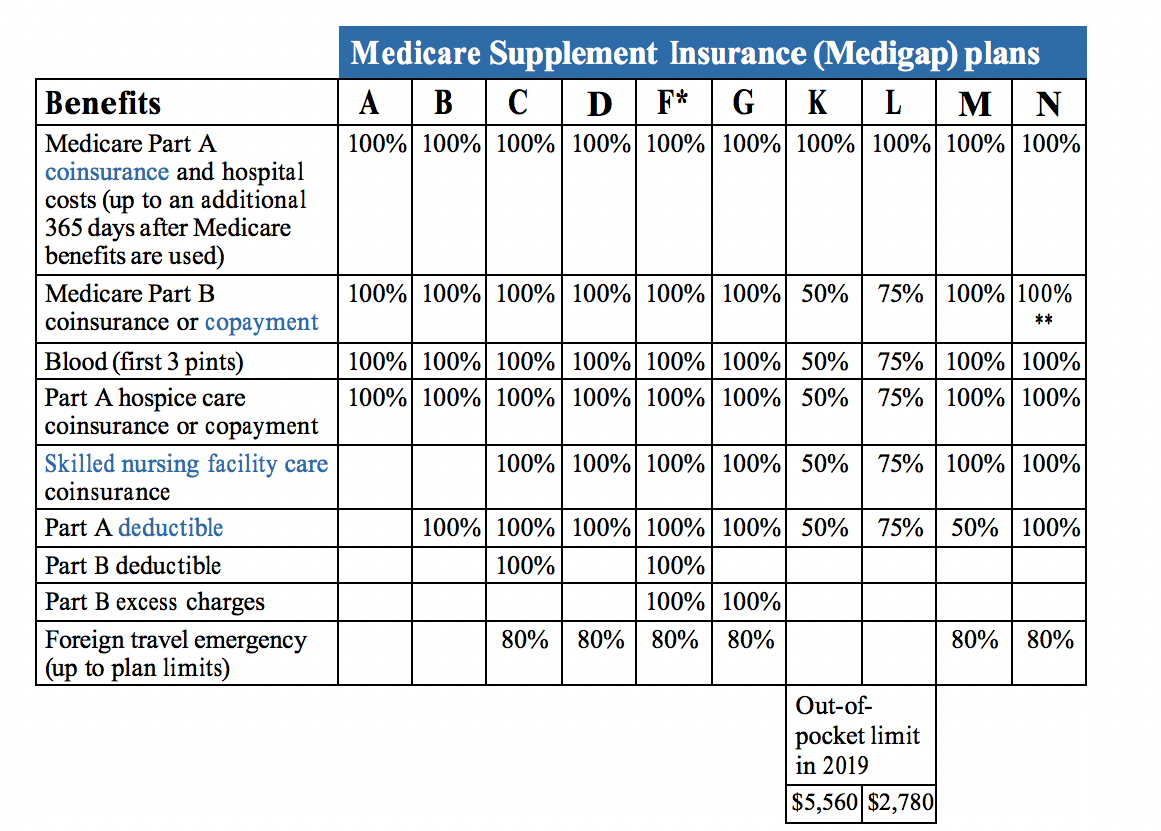
Prescription drug benefits refer to getting a specific option under a companys health insurance coverage that allows individuals covered by the plan to get any prescription medication needed. Member pays 30 per Prescription Benefit Plan RX 2 Only available with Medical Plans A B D F G H J K L M O P T U V X Y Z Retail 30day supply. Learn more about the coverage and benefits offered by Aetnas pharmacy plans including prescription drug.
You can fill prescriptions for the medications you take regularly also called long-term or maintenance medications in 90-day supplies. This deductible is separate from the Plans calendar year deductible. Please be sure to look at your Paramount ID card to determine if you are covered for prescriptions.
Get to know your Express Scripts pharmacy benefits. Prescription benefits are administered by the health plans prescription benefit manager PBM. Most of our employer group members have drug coverage as part of your insurance with us.
Our prescription benefit plan consists of a coherent and cohesive assembly of concepts products and services. It applies only to prescriptions that you buy at any network or out-of-network retail drugstore or pharmacy. You take the card and your prescription which must be written on your Physicians prescription pad to a Participating Pharmacy.
The need for a prescription drug benefit plan.