Both group insurers and HMOs must provide infertility treatment coverage of IVF uterine embryo lavage embryo transfer artificial insemination GIFT ZIFT low tubal ovum transfer and more but coverage of IVF GIFT and ZIFT is only provided if other less costly treatments havent been successful. What that means is if your health plan didnt cover fertility treatments before the ACA became law in 2010 it doesnt have to cover them now.
 Fertility Insurance Coverage Benefits Tampa Fl The Reproductive Medicine Group
Fertility Insurance Coverage Benefits Tampa Fl The Reproductive Medicine Group
However Blue Cross Blue Shield is a national federation of.
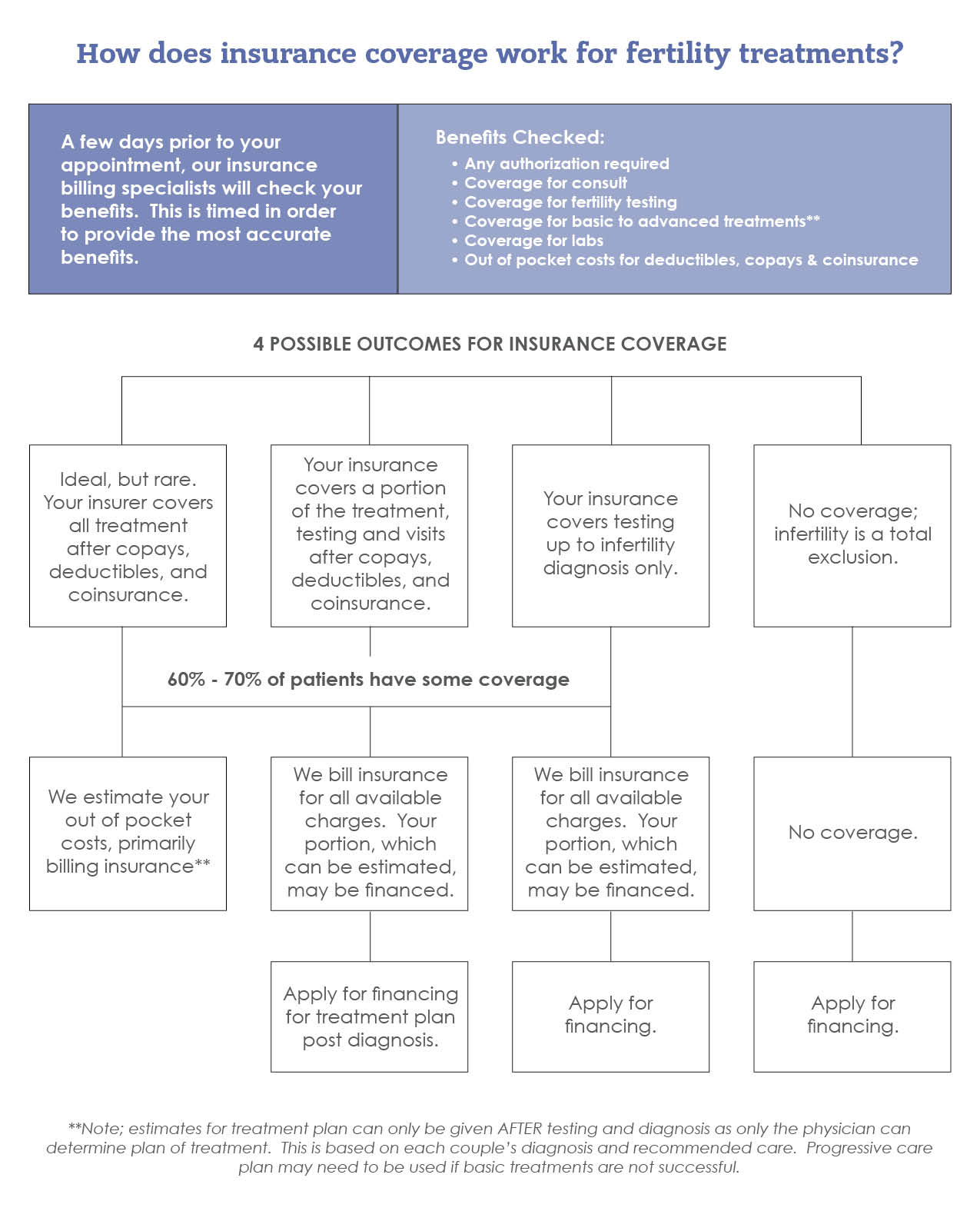
Insurance plans that cover infertility treatments. Health Insurance that covers Infertility Treatment. In some states religious organizations are also allowed to opt out of coverage. Assessing health insurance benefits for fertility treatment coverage.
Keep in mind that these mandates typically only apply to employer-sponsored plans. The National Infertility Association argues that infertility and fertility treatments are reproductive healthcare in the same way that pregnancy prevention is reproductive healthcare. Blue Cross Blue Shield BCBS will sometimes issue plans that cover infertility treatment including IVF when required by state law or when requested by an employer group.
Blue Cross Blue Shield PPO. IVF with embryo transfer that involves an IVF cycle resulting in embryo implantation is regarded as an IVF attempt as per coverage policy. These plans usually pay for diagnostic tests for infertility treatments.
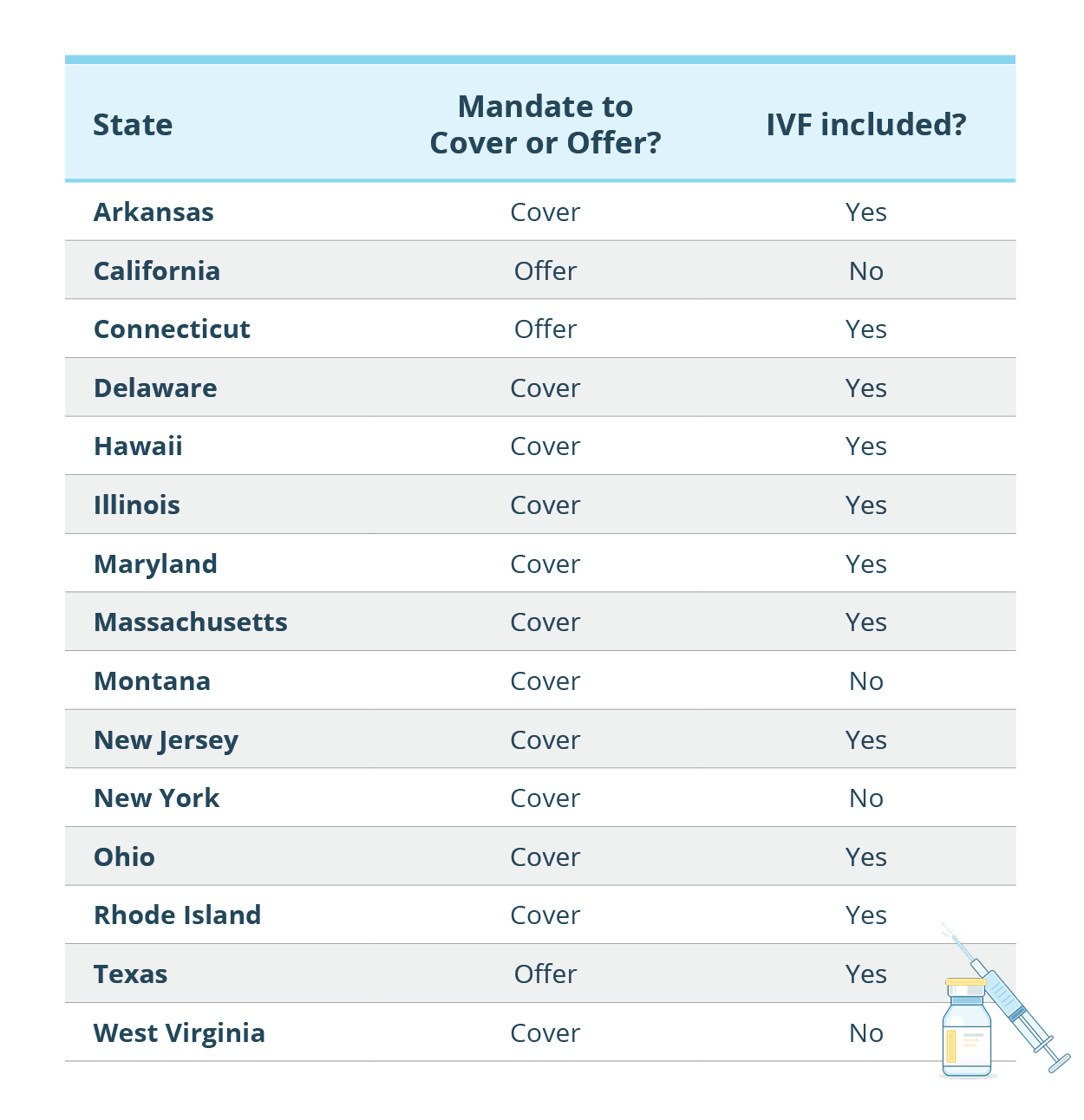
For instance some states require all plans to help pay for infertility treatments a mandate to cover while others only require insurers to offer one plan with infertility benefits mandate to offer. 91 Enter Mobile Number. Treatments include hormone management injectable endocrine therapies surgical interventions and artificial insemination.
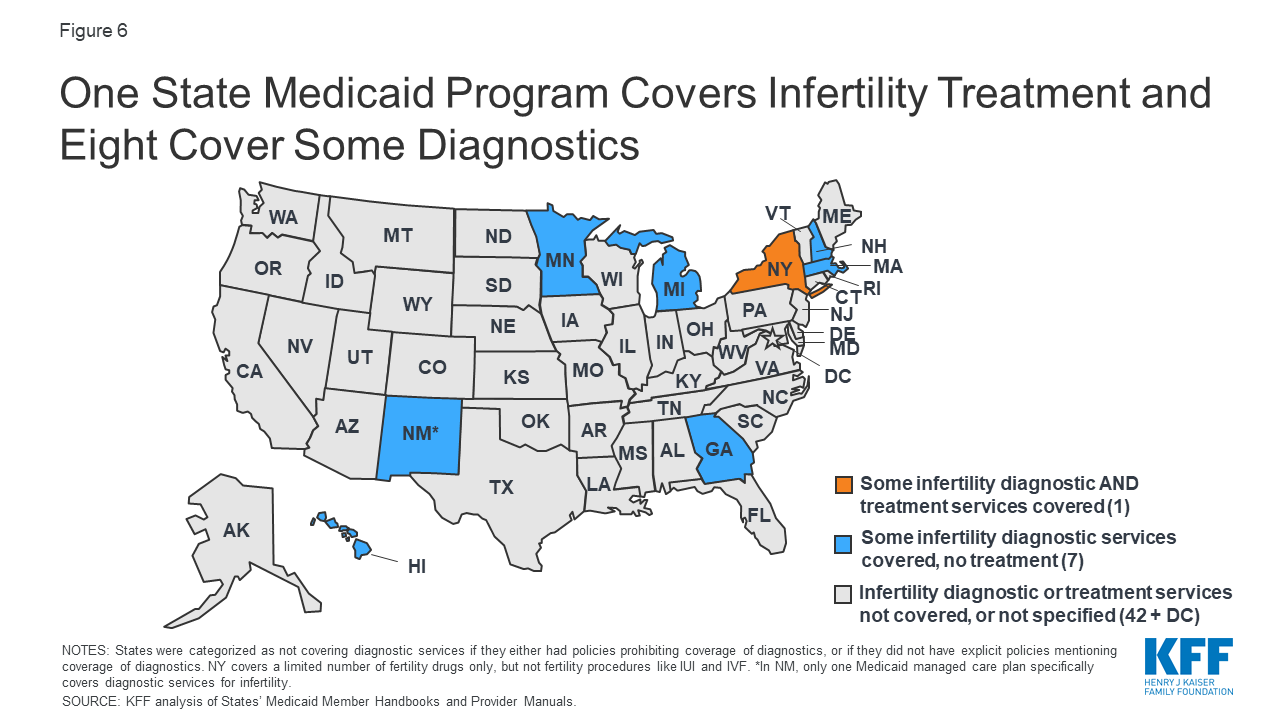
Additionally there are seven states that legislate that insurance plans must cover treatments for folks whose infertility is medically induced ie. Additional embryo implantations are considered subsequent IVF. Under this policy the insurance company shall pay medical expenses if you are hospitalized on the advice of a medical practitioner for infertility or subfertility treatments.
Once infertility has been established Cigna will offer coverage for specific treatments if the member owns a plan which covers them. Infertility is a medical concern just like any other so activists want to know why it isnt covered by insurance like any other. IVF treatments alone cost on average 10000 and the related drugs can cost an additional 7000 or more.
IVF1 accepts the following insurance plans covering the cost of infertility treatment. Unfortunately the treatment is expensive and not guaranteed to work. Digit Health Insurance covers Accidental Illness COVID-19 Hospitalization.
In certain states insurers are legally required to offer infertility coverage but this requirement looks different in every state. Manulife is one of the Canadian insurers that offer plans to cover fertility drugs associated with IVF treatments. The law requires every plan to communicate the availability of coverage to group contractholders.
Up to six egg retrievals are also covered. Our physicians also promote the extension of healthcare insurance to cover more infertility treatments and costs by negotiating with individual insurance plans and engaging in the discussion of adopting mandated coverage at the state and federal levels. Living in a state with an infertility mandate will help the case.
The law defines infertility treatment for infertility. Blue Cross Blue Shield. Short-term disability is the first form of supplemental health insurance for women undergoing infertility treatments including In Vitro Fertilization.
Eligibility The Digit Health Insurance plan offers Infertility Treatment cover as an add-in cover that one can opt for. There is also legislation that requires companies to offer health insurance policies that cover infertility treatments available but they dont require employers to cover infertility treatment costs. Barbara Collura of Resolve.
Although Obamacare requires health insurance companies to cover 10 categories of services known as essential health benefits infertility treatment is not one of them. Insurance Code 101196 require specified group health care service plan contracts and health insurance policies to offer coverage for the treatment of infertility except in vitro fertilization. Blue Cross Blue Shield HMO.
Depending on location plans may cover IVF. Aetna plans may cover diagnostic infertility services such as laboratory studies imaging studies biopsies and physical examinations. Health Safety Code 137455 and Cal.
Apply for a new policy before your next cycle. Members you want to insure Members you want to insure. Request an online quote Sponsored Link and connect with an agent licensed in your state.
In the treatment of unexplained infertility ART procedures like IVF are pursued. States that provide these options include California Louisiana Montana Ohio Texas and West Virginia. The good news is that nearly every major medical insurance provider does offer some type of infertility treatment coverage.
This coverage fills the lost income gap found in all primary policies. Insurers and HMOs that cover pregnancy benefits must provide coverage for medically necessary expenses of diagnosis and treatment of infertility and for standard fertility preservation services when a medically necessary medical treatment may directly or indirectly cause iatrogenic infertility to a covered person. A particular brand of insurance is not indicative of whether or not your infertility treatment care is covered by your carrier because every insurance company offers a variety of plans.
From chemotherapy radiation surgery or other medical care that compromises fertility.