Blue Cross and Blue Shield of Louisiana an independent licensee of the Blue Cross and Blue Shield Association offers Blue Advantage PPO. Vermont Blue Advantage is a PPO and HMO plan with a Medicare contract.
Https Www Bcbstx Com Provider Pdf Hmo Sec B A Network Id Pdf
Blue Advantage from Blue Cross and Blue Shield of Louisiana HMO is an HMO plan with a Medicare contract.
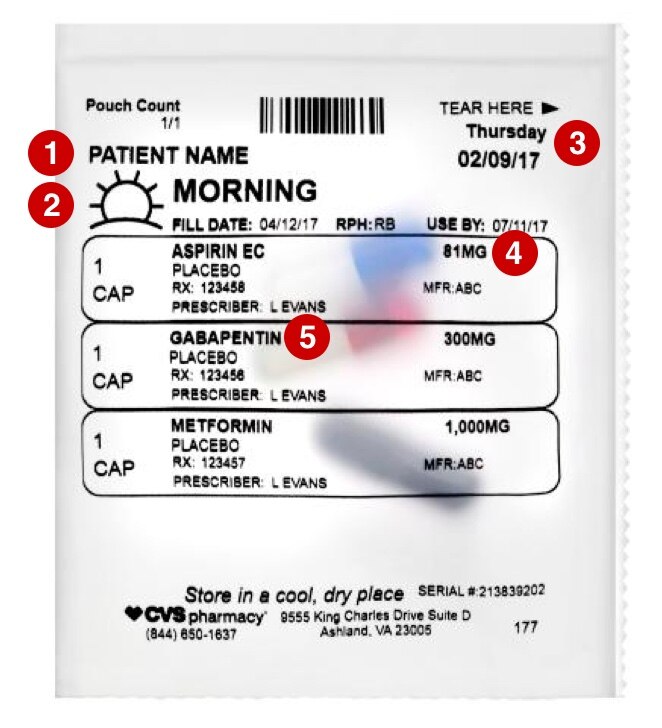
What is blue advantage hmo. 200 from Blue Cross and Blue Shield of Texas. If you require services that are not available from a specialist within the Wellmark Blue HMO Network you will be referred to a provider outside the Wellmark Blue HMO Network who has expertise in diagnosing and treating your condition. Blue Advantage HMO members will continue to use BlueAdvantage HMO contracted providers for medical eye care.
It was developed for individuals under the age. BlueAdvantage HMO offers one of the largest provider networks of primary care physicians PCPs and hospitals in the state. Please include all appropriate diagnosis codes on your claims in order to accurately represent the services.
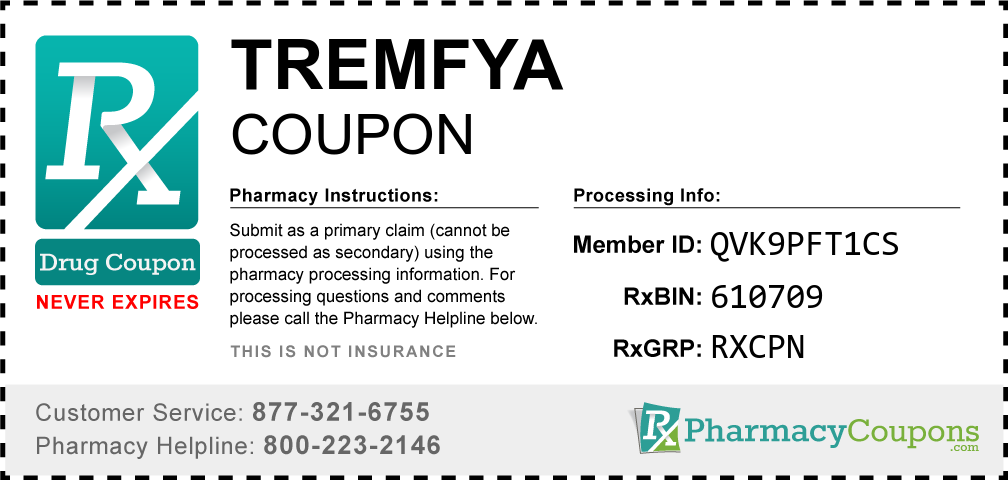
This formulary was updated on 4202021. Blue Advantage HMO members 19 and younger will receive their annual eye exam and eye wear from EyeMed Vision Care providers. Blue Cross Blue Shield offers several types of Medicare Advantage plans including.
Learn more about plan monthly costpremimum deductiblesprescription drug coverage hospital services accepted doctors and more. BLUE ADVANTAGE A Blue Cross HMO a product of Blue Cross and Blue Shield of Illinois HMO. Get Health Insurance plan info on Blue Advantage Security HMO.
To that end Florida Blue developed a different type of HMO product called. MyBlue is a Different Type of HMO Product. HMO products underwrHMO Nevada.
Medicare beneficiaries may also enroll in Vermont Blue Advantage through the CMS Medicare Online Enrollment Center located at httpswwwmedicaregov. Wellmark must approve out-of-network referrals before you receive services or the services will. Blue Advantage from Blue Cross and Blue Shield of Louisiana is a PPO plan with a Medicare contract.
With 16 billion in revenue and more than 12 million plan members across the country Anthem Blue Cross and Blue Shield is proud to carry on the tradition of bringing you the health plans you prefer from a company you can count on. Itten by HMO Colorado Inc. Enrollment in Vermont Blue Advantage depends on contract renewal.
A HMO or Health Maintenance Organization is a type of Medicare Advantage MA or Part C plan. This cost-effective network is designed to provide affordable quality health care services to the uninsured and underinsured. Blue Advantage from Blue Cross and Blue Shield of Louisiana is a PPO plan with a Medicare contract.
You can see our. The BlueAdvantage HMO plan is brought to you by HMO Colorado Inc a subsidiary of Anthem Blue Cross and Blue Shield. Both are independent licensees of the Blue Cross and Blue Shield Association.
These plans are made up of regional networks of doctors hospitals and specialists who all agree to. Blue Advantage HMO Blue Advantage PPO has a network of doctors hospitals pharmacies and other providers. For more recent information or other questions please call Blue Advantage Customer Service.
Blue Cross and Blue Shield of Texas BCBSTX is pleased to offer our Blue Advantage HMO and Blue Advantage Plus HMO network in all 254 Texas counties. Anthem Blue Cross and Blue Shield is the trade name of Rocky Mountain Hospital and Medical Service Inc. If you use the providers that are not in our network the plan may not pay for these services.
Enrollment in either Blue Advantage plan depends on contract renewal. Enrollment in either Blue Advantage plan depends on contract renewal. Blue Cross and Blue Shield of Louisiana HMO offers Blue Advantage HMO.
Search for Doctors and Hospitals. Blue Advantage HMO members must use plan providers except in emergency or urgent care situations. The Pathway HMO network does not include all providers in the HMO Nevada managed care network.
HMO plans always offer the same benefits as any other Medicare plan but they are also able to provide additional benefits many plans include vision dental and. See the Pathway HMO directory for a complete. You must generally use network pharmacies to fill your prescriptions for covered Part D drugs.
Our products and services are continually evolving to ensure we stay true to our mission of helping people and communities achieve better health. The Office of Personnel Management has determined that the BlueAdvantage HMO on the Pathway HMO Network prescription drug coverage is on average expected to pay out as much as the standard Medicare prescription drug coverage will pay for all plan participants and is considered Creditable Coverage. Free gift without obligation to enroll.



/ScreenShot2021-02-11at3.31.52PM-d4cdbd3f5e984eebb91c2b0478e46dc2.png)