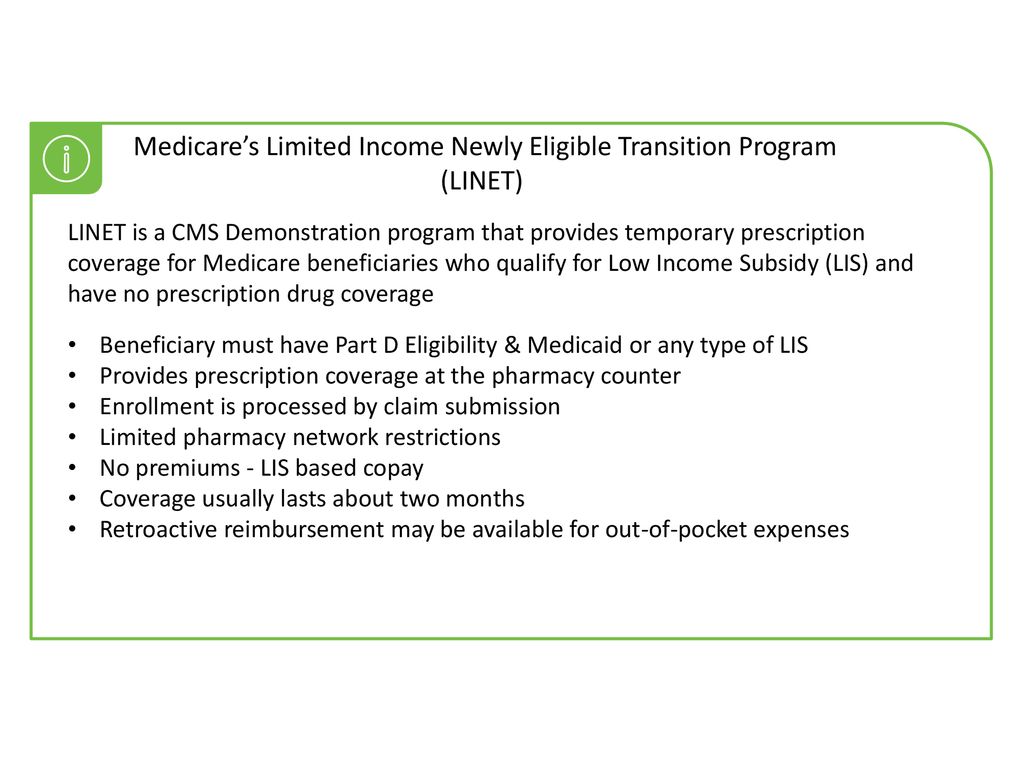
Transition Program LI NET Program overview LI NET is a demonstration program created by the Centers for Medicare Medicaid Services CMS to eliminate gaps in prescription drug coverage for low-income Medicare beneficiaries It is designed for those who qualify for Low Income Subsidy LIS. To enroll in LINET.
 Cms Programs Targeting Beneficiaries With Low Income Or Otherwise Dually Eligible 8 22 Ppt Download
Cms Programs Targeting Beneficiaries With Low Income Or Otherwise Dually Eligible 8 22 Ppt Download
30 days maximum supply.
Linet prescription program. LINET Enrollment Form LINET is a Center for Medicare Medicaid Services CMS demonstration program that provides temporary prescription coverage for Medicare beneficiaries who qualify for l ow-income subsidy LIS and have no prescription drug coverage. Medicare Part D is an optional benefit. LINET LINET is a CMS Demonstration program that provides temporary prescription coverage for Medicare beneficiaries who qualify for Low Income Subsidy LIS and have no prescription drug coverage Beneficiary must have Part D Eligibility Medicaid or any type of LIS Provides prescription coverage at the pharmacy counter.
The LI NET Program ensures that individuals with Medicares low-income subsidy LIS or Extra Help who are not yet enrolled in a Part D prescription drug plan are still able to obtain immediate prescription drug coverage. LI NET provides immediate point-of-sale prescription drug coverage for people with LIS Extra Help who are NOT YET ENROLLED in a Part D plan. In 2018 the LINET program.
LI NET will help you pay for covered prescriptions you filled from 01012018 until 01312018. The Limited Income Newly Eligible Transition LI NET Program. This is a special prescription drug program administered by Humana which temporarily covers your drug needs until you choose a Medicare Part D plan or you are automatically enrolled into a Medicare Drug plan.
Currently the LINET demonstration program provides temporary Medicare Part D coverage and cost-sharing assistance for newly-eligible low-income Medicare beneficiaries. Tion Program LINET to provide immediate medication access for Medicare beneiciaries with Extra Help also known as the Low-income Subsidy or LIS not yet enrolled in a Part D plan or a Medicare Advantage Part C plan with prescription drug coverage. Coverage for people who qualify for Medicares low-income subsidy LIS also called Extra Help and are eligible for.
8 2018 Medicares LI NET program will limit the supply for prescription drugs to no more than a 60-day supply per fill. LI NET has an open formulary and contains all Part D drugs. All enrollees are temporarily covered until they are enrolled in a Part D.
The maximum supply for the following scenarios will remain the same. Full Benefit Dual Eligible and SSI-Only beneficiaries on a retroactive basis up to 36 months in the past. Every older American who needs prescription drug coverage is able to access and afford it regardless of their income.
Limited Income Newly Eligible Transition LINET Changing a Prescription Drug Plan. Refunds from Part D Plans. The LI NET Program ensures that individuals with Medicares low-income subsidy LIS or Extra Help who are not yet enrolled in a Part D prescription drug plan are still able to obtain immediate prescription drug coverage.
LINET is a CMS demonstration program that provides temporary prescription coverage for Medicare beneficiaries who qualify for low-income subsidy LIS and have no prescription drug coverage Enrollment methods AUTO-ENROLLED Periodic enrollments by CMS POINT OF SALE Enrolled by claim submission RETROACTIVE Reimbursement request. CMS awarded the LINET program contract to Humana. Beneficiaries may be qualified for a Retroactive Reimbursement coverage for months that they were not on a Part D plan and retroactive coverage paid out of pocket.
Medicares Limited Income NET Program. If an individual is later determined to be ineligible because. Point-of-sale prescription drug coverage.
Tion Program LINET to provide immediate medication access for Medicare beneiciaries with Extra Help also known as the Low-income Subsidy or LIS not yet enrolled in a Part D plan or a Medicare Advantage Part C plan with prescription drug coverage. Medicares Limited Income NET Program for people with retroactive Medicaid SSI eligibility Medicares Limited Income NET LINET Program provides temporary drug. To receive Medicare Part D coverage a.
The Limited Income Newly Eligible Transition LI NET Program provides immediate temporary medication access for Medicare beneficiaries newly receiving Extra Help who lack a prescription drug plan. Medicare Part D is a prescription drug program for persons who are eligible for Medicare Part A or Medicare Part B. 30 days maximum supply.
Medicares Limited Income NET Program effective January 1 2010 provides temporary Part D prescription drug coverage for low income Medicare beneficiaries not already in a Medicare drug plan including. The prescription below details LINET eligibility requirements and enrollment processes which. Use the 4Rx data in the patients enrollment.
Immediate need prescription drug coverage. What is Medicare Part D. Frequently Asked Questions The Centers for Medicare Medicaid Services CMS created the Limited Income Newly Eligible Transition LI NET Program to provide immediate temporary medication access for low-income Medicare beneficiaries without prescription drug coverage.
CMS awarded the LINET program. Individuals must not be enrolled in any other Medicare Part D prescription drug plan and must have either Medicare and Medicaid or Medicare and the Low-Income Subsidy LIS. 34 days maximum supply.